A new study from researchers at the University of Alabama at Birmingham is shining a light on the similarities and differences between COVID-19 and H1N1 influenza, and how they both affect the lungs in severe cases.
In the study, published in March 2021, postdoctoral researcher Camilla Margaroli in the laboratory of Amit Gaggar, M.D., in the UAB Division of Pulmonary, Allergy and Critical Care, says while the COVID-19 pandemic reached critical severity worldwide, many patients developed rapidly progressive respiratory failure, a particular form of lung injury that often requires ICU-level care, mechanical ventilation and prolonged in-hospital stays and has a high associated mortality.
“Similar to COVID-19, influenza has led to a number of worldwide pandemic outbreaks, and the most severe cases of flu require the same level of care as severe COVID-19 patients,” Margaroli said. “Therefore, understanding differences and similarities between these two viral infections could improve patient care, as well as identify novel therapeutic targets.”
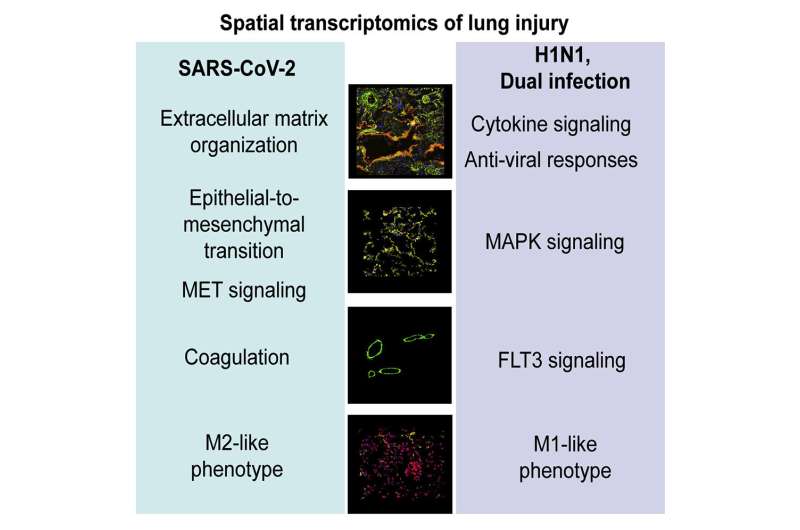
To address this question, Margaroli and her team used a cutting-edge technique called spatial transcriptomics, that allows for the identification of genetic responses while maintaining the tissue architecture intact, thus reducing the risk of processing-induced changes.
“We found that, even though both viral infections may require ICU-level care for the most severe cases, there were striking differences in how the lung responded to these two viruses,” she said.
COVID-19 patients developed a response that would induce the remodeling of the lung tissue, which would make this organ more stiff and therefore harder to breathe. These changes were translated in the adaptation of the individual cell types that compose the lung: epithelium, vasculature and macrophages, which are a type of immune cell that resides in the lungs and coordinates the inflammatory response.
These new findings define a unique tissue response to SARS-CoV-2 and may open opportunities for novel targeted therapeutic approaches for both COVID-19 and influenza patient groups. They also provide a new platform to study other common severe illnesses where organ injuries are present.
Source: Read Full Article
