Over the course of the COVID-19 pandemic, scientists have strived to answer basic questions about the amount of SARS-CoV-2 virus required to cause an infection and how that viral dose influences disease severity. Answers to these questions help drive public health decisions to keep public spaces safe and serve as the foundation for future COVID-19 research.
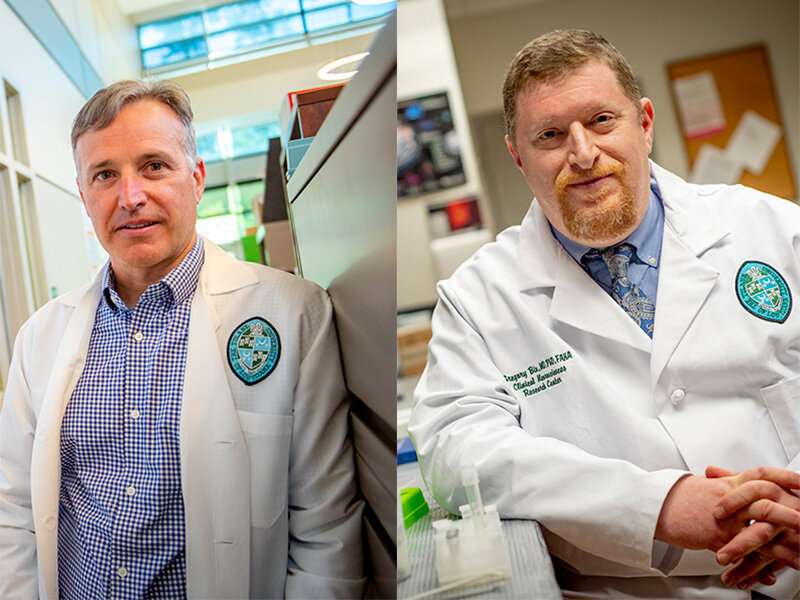
Tulane researchers Chad Roy, Ph.D., and Dr. Gregory Bix were among a group of scientists who co-authored a review of 115 peer-reviewed studies to identify gaps in current knowledge and suggest opportunities for future research into SARS-CoV-2 and COVID-19. Their conclusions were published in Clinical Infectious Diseases.
Understanding how SARS-CoV-2 is transmits from one person to another has been key to halting its spread. This review found that the virus is primarily transmitted through the inhalation of particles containing virus (not through contact surfaces), and that the ability of those particles to infect is dependent both on the environment and the unique physiology of the individual. Concentration of viral particles plus the length of time one is in contact with those particles ultimately determines one’s exposure.
Importantly, the team concluded that the viral dose, or amount of infectious virus transmitted from one person to another, does not appear to affect disease severity. In practical terms, this means that an individual who inhales a greater number of infectious particles will not necessarily experience more severe disease than an individual who is infected with a smaller amount. However, the likelihood of becoming infected may rise with the size of that “dose.” The review concluded that some interventions, such as the practice of wearing face masks, can reduce the risk of infection by reducing exposure but would likely not affect severity of disease if infected.
Roy, professor of microbiology and immunology and director of infectious disease aerobiology at the Tulane National Primate Research Center, believes that the more important factor in determining disease severity is the unique vulnerabilities of the host, or the person that becomes infected.
“While we are still learning a lot about the size of the dose required to induce infection, it’s apparent that the relationship between an individual and the virus dictates disease severity more than the size of the dose,” Roy said.
Throughout the pandemic, one of the most vexing concerns is why some people get so sick while others are asymptomatic. While disease severity is associated with older age, male sex, certain comorbidities and smoking, the authors also note that neither lack of comorbidities nor younger age guarantee mild disease, and that much is yet to be learned about what makes certain individuals susceptible to severe disease and death. “Long COVID” or symptoms that linger long after the acute period of illness is still being investigated as data continues to accrue.
Bix, professor and vice chair of neurosurgery and neurology, director of COBALT (COVID-19 biobank and library at Tulane), and director of the clinical neuroscience research center, concludes that the key to better understanding COVID disease outcomes lies in increasingly refined pre-clinical and epidemiologic studies.
Source: Read Full Article
