Study Links Placental Group B Streptococcus to Higher Neonatal Unit Admissions in Newborns

In a recent study published in Nature Microbiology, a group of researchers investigated the clinical significance of Streptococcus agalactiae (Group B Streptococcus; GBS) deoxyribonucleic acid (DNA) in the placenta in relation to neonatal unit (NNU) admission and morbidity in term infants.
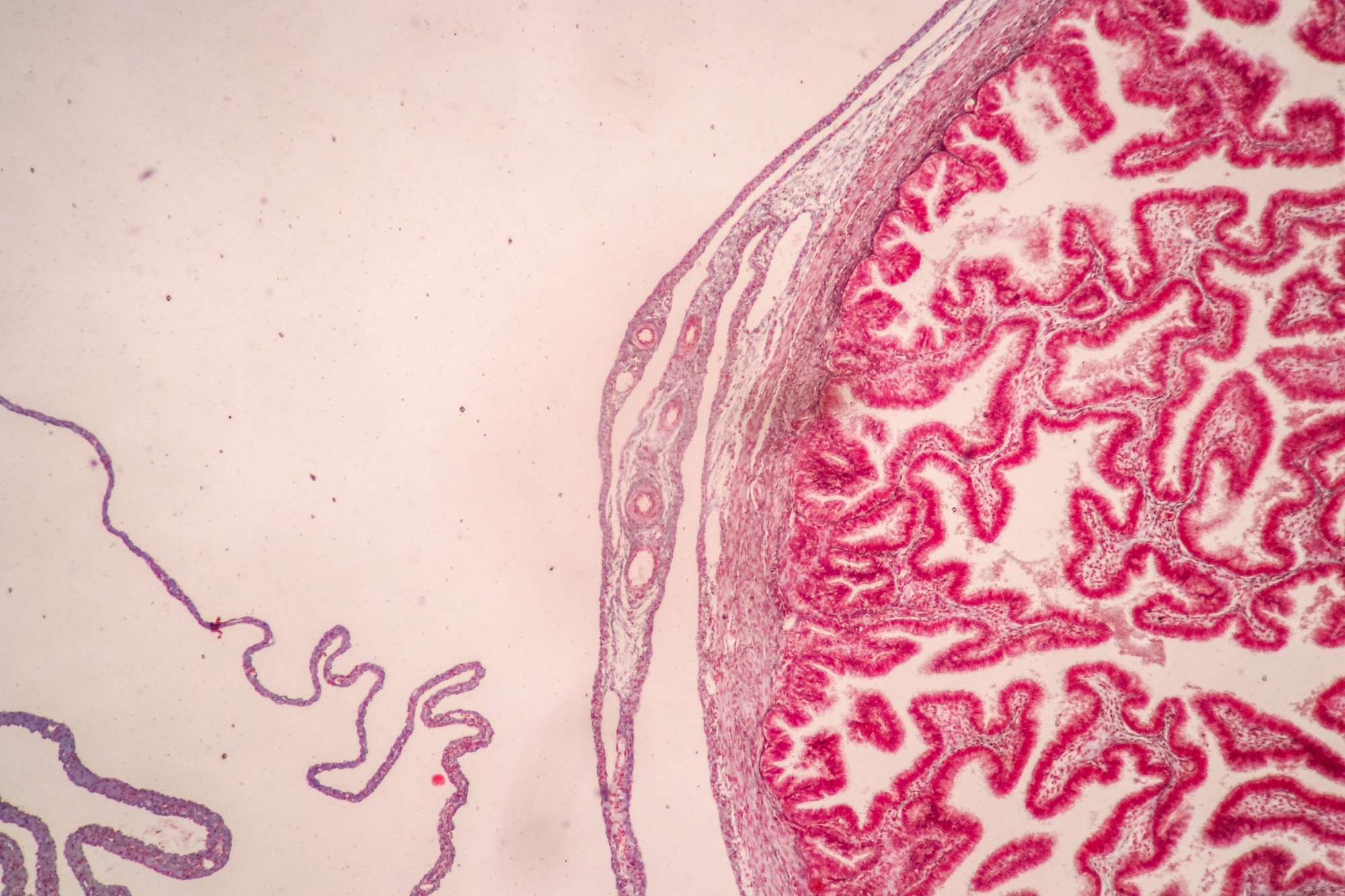 Study: Placental Streptococcus agalactiae DNA is associated with neonatal unit admission and foetal pro-inflammatory cytokines in term infants. Image Credit: Rattiya Thongdumhyu/Shutterstock.com
Study: Placental Streptococcus agalactiae DNA is associated with neonatal unit admission and foetal pro-inflammatory cytokines in term infants. Image Credit: Rattiya Thongdumhyu/Shutterstock.com
Background
GBS is the common cause of neonatal sepsis in the first week of life, known as early-onset disease (EOD). About 20% of women carry GBS in their genital tract, and without intervention, around 1% of infants from these women develop EOD.
In 2020, about 20 million pregnant women were GBS carriers, leading to 230,000 cases of EOD and contributing to roughly 50,000 stillbirths and 50,000-100,000 infant deaths globally. In high-income countries, EOD is a rare phenomenon, while it occurs fairly often in low-income countries, although the data is less precise.
Previous metagenomics research identified GBS as the sole bacteria in the placenta before labor in term pregnancies. Further research is needed to fully understand the mechanisms by which GBS presence in the placenta leads to neonatal morbidity and to develop targeted interventions for prevention and treatment in diverse global settings.
About the study
The present study utilized data and samples from a prospective cohort of unselected nulliparous females with a single pregnancy who received antenatal care at the Rosie Hospital in Cambridge, United Kingdom (UK), from 2008 to 2013.
The only exclusion criterion was multiple pregnancies. Women were recruited around the time of their dating ultrasound scan, typically at around 12 weeks of gestation, and were followed up with research visits at 20, 28, and 36 weeks of gestational age.
After delivery, technicians systematically sampled the placenta, umbilical cord, and fetal membranes. These samples were immediately flash-frozen for molecular analysis and fixed for microscopy. Additionally, umbilical cord blood was collected from approximately a third of the participants.
Outcome data for the study were thoroughly compiled, including individual examination of the mother's medical records and linkage to various electronic databases containing clinical information, with results from all microbial cultures performed during the pregnancy.
A pregnancy outcome prediction (POP) study was conducted with a sample size of 4,212 women. The height, median age, body mass index (BMI), and interquartile ranges were recorded.
Ethical considerations were followed in the research, which the Cambridgeshire 2 Research Ethics Committee approved with reference number 07/H0308/163. Informed consent was obtained from all of the participants in written form, and the ethical requirements were followed.
Study results
In this reanalysis, the focus was on 436 term fetuses who were cases defined by admission to an NNU within 48 hours and beyond 48 hours after delivery. The results showed that 23.3% of term infants with placental GBS DNA and 8.4% without were admitted to the NNU.
This indicated a significant association between placental GBS DNA and NNU admission, even after adjusting for maternal characteristics.
This was followed by another validation study involving non-overlapped 239 cases of term NNU admissions and 686 term control groups obtained from the same cohort. The present study replicated the results of the first one, revealing the linkage of placental GBS DNA with the rising prevalence of NNU admissions.
Further analysis distinguished septic from non-septic phenotypes of neonatal morbidity. This study categorized NNH admissions according to clinical proof of sepsis, from none to confirmed GBS sepsis.
Placental GBS was significantly associated with admissions into NNU, where probable, culture-negative, and proven GBS sepsis were considered outcome measures. Pathological findings on the fetal membranes and umbilical cord were strongly associated with placental GBS DNA in cases accompanied by chorioamnionitis and funisitis.
The other aspect that the study looked at is the rates of placental GBS associated with genital tract colonization. It found a higher prevalence of GBS-positive placentas in participants with a positive high vaginal swab (HVS) for GBS during pregnancy compared to those with a negative HVS or no HVS culture.
The researchers also showed no association between the detection of GBS DNA in the placenta and the timing of births or methods of deliveries. Moreover, additional tests to certify the GBS DNA sign, involving novel reverse transcriptase- quantitative polymerase chain reaction (RT- qPCR) assay for GBS 16S ribosomal ribonucleic acid (rRNA), proved that such findings were reliable.
Analysis of pro-inflammatory cytokines in umbilical cord serum from term births with GBS-positive placentas revealed a 'cytokine storm' – a significant elevation of cytokines – compared to GBS-negative cases. This suggested an exaggerated inflammatory response to the pathogen.
Finally, the study detailed the clinical features of cases with proven and probable GBS sepsis. It found that only a minority of these cases had GBS colonization detected antenatally or received antibiotics in labor.
This emphasized the potential under-recognition of GBS-related neonatal morbidity and the need for better screening and prophylactic measures. The presence of GBS DNA in the placenta is strongly associated with an increased risk of neonatal morbidity, evidenced by NNU admission.
This association was not only consistent across different analytical methods but also highlighted the potential for an exaggerated inflammatory response in neonates, leading to severe outcomes.
The study's findings have significant implications for clinical practice, particularly concerning the screening and treating GBS in pregnant women.
-
Gaccioli, F., Stephens, K., Sovio, U. et al. (2023) Placental Streptococcus agalactiae DNA is associated with neonatal unit admission and foetal pro-inflammatory cytokines in term infants. Nat Microbiol., doi: https://doi.org/10.1038/s41564-023-01528-2. https://www.nature.com/articles/s41564-023-01528-2
Posted in: Child Health News | Medical Science News | Medical Research News | Women's Health News
Tags: Assay, Bacteria, Blood, Body Mass Index, Cytokine, Cytokines, DNA, Hospital, Labor, Metagenomics, Microbiology, Microscopy, Pathogen, Placenta, Polymerase, Polymerase Chain Reaction, Pregnancy, Research, Reverse Transcriptase, Ribonucleic Acid, Sepsis, Ultrasound, Umbilical Cord, Vaginal

Written by
Vijay Kumar Malesu
Vijay holds a Ph.D. in Biotechnology and possesses a deep passion for microbiology. His academic journey has allowed him to delve deeper into understanding the intricate world of microorganisms. Through his research and studies, he has gained expertise in various aspects of microbiology, which includes microbial genetics, microbial physiology, and microbial ecology. Vijay has six years of scientific research experience at renowned research institutes such as the Indian Council for Agricultural Research and KIIT University. He has worked on diverse projects in microbiology, biopolymers, and drug delivery. His contributions to these areas have provided him with a comprehensive understanding of the subject matter and the ability to tackle complex research challenges.