MILAN — When added to prostate biopsy, gallium-68 prostate-specific membrane antigen (PSMA)-PET/CT improves detection of clinically significant prostate tumors and helps guide treatment planning, new research shows.
An interim analysis of the DEPROMP trial revealed that, compared with the standard of care, the addition of PSMA-PET/CT-targeted biopsy to multiparametric MRI led to a change in intramodal treatment plans, such as the decision to use a nerve-sparing approach or a change regarding the extent of lymph node dissection, as well as decisions regarding intermodal approaches, such as the use of local vs systemic therapy, in more than half of cases.
The addition of PSMA-PET/CT also slightly increased diagnoses of clinically significant cancers, according to data presented at the recent European Association of Urology (EAU) 2023 Annual Meeting.
“PSMA-PET/CT seems to influence our actions during prostate cancer diagnosis,” said Phillip Krausewitz, MD, from University Hospital Bonn, in Bonn, Germany, who highlighted the findings during an oral abstract presentation at the EAU meeting.
Krausewitz cautioned, however, that the results are preliminary and are based on the first 100 patients enrolled in the study, and that data on the planned cohort of 230 patients may better elucidate the additive effects of PSMA-PET/CT.
Several experts also noted that including PSMA-PET/CT in primary prostate cancer staging adds considerable costs, which may be a barrier to its wide adoption.
“In 2023, it’s not a practical screening tool, given its very, very high costs,” Mark Pomerantz, MD, of the Dana-Farber Cancer Institute in Boston, told Medscape Medical News.
Inside the Analysis
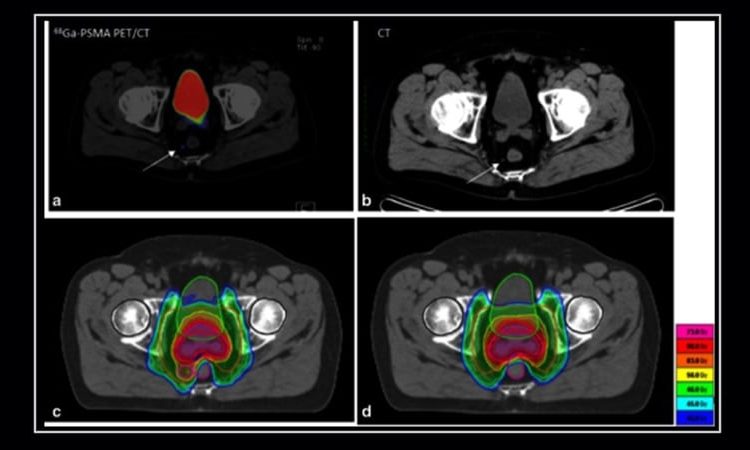
PSMA-PET/CT has already been shown to improve detection of prostate cancer metastasis and local T-staging in combination with MRI.
In the current analysis, Krausewitz and colleagues wanted to know whether the value of PSMA-PET/CT extended to prostate biopsy diagnostics.
In the prospective DEPROMP trial, 230 biopsy-naive men with suspected prostate cancer underwent MRI and PSMA-PET/CT fusion biopsy, which included undergoing both systematic and targeted biopsies of suspicious lesions.
On the basis of these findings, risk stratification and patient management plans were developed. Patient records were randomly assigned to different evaluation teams: one team received all results, including findings from PSMA-PET/CT-guided biopsy, and one team received the MRI findings. The subsequent management plans, developed by independent urologists, were then compared.
Krausewitz presented data on the first 100 patients enrolled; 56 of the patients had been diagnosed with prostate cancer, and 44 of the patients had not been diagnosed.
Compared with standard of care, the addition of PSMA-PET/CT-targeted biopsy led to changes in intramodal and intermodal approaches in 53% of cases. Among patients with clinically significant prostate cancer, the added information gleaned from PET/CT changed the treatment proposal in 85% of men.
The addition of PSMA-PET/CT also resulted in a 3% increase in diagnoses of clinically significant cancers and a 1% decrease in detection of nonsignificant cancers.
“Based on our interim analysis, the conclusion can be drawn that PSMA-PET/CT seems to slightly increase the detection rate of clinically significant prostate cancer during prostate biopsy, and it is not inferior to MRI fusion biopsy,” Krausewitz said.
However, experts not involved in the researcher expressed uncertainty about the broader use of the technology.
PSMA-PET/CT is “very good at detecting very small tumors, including tumors that are making PSAs [prostate-specific antigen levels] of less than 1 [ng/mL], and in theory, it could be helpful one day in screening for the disease,” but it “hasn’t been extensively studied as a screening tool,” said Pomerantz.
It’s still unknown, however, what the false positive rate is and whether the technology could lead to overtreatment as a result of “chasing after every little shimmer of light on one of those PSMA scans,” he said.
The cost of adding PSMA-PET/CT compared with standard of care is also likely to be a significant barrier to its wider use, Pomerantz added.
Jochen Walz, MD, associate professor of Urology at the Institut Paoli-Calmettes Cancer Centre in Marseille, France, agreed about the costs of PSMA-PET/CT. He noted that investigators would have to show that it offers substantial advantages over MRI-guided biopsy before it could be more widely adopted.
“In the meantime, PSMA-PET/CT could be considered a solution for selected challenging diagnostic cases or those where MRI cannot be done,” Walz said.
The DEPROMP Trial is funded by the Commission of Clinical Studies of the Medical Faculty of the Rheinische Friedrich-Wilhelms-University Bonn and the University Hospital Bonn’s Department of Urology. Krausewitz is an employee of the University of Bonn. Pomerantz and Walz have disclosed no relevant financial relationships.
European Association of Urology (EAU) 2023 Annual Meeting: Abstract A0056. Presented March 10, 2023.
Neil Osterweil, an award-winning medical journalist, is a long-standing and frequent contributor to Medscape.
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article