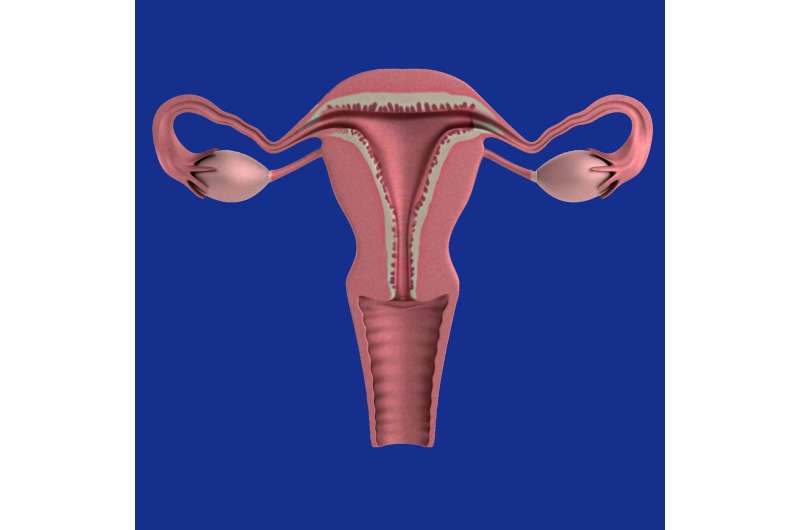
Endometriosis is a debilitating disease that affects an estimated one million Canadians. It involves the overgrowth of endometrial tissue (the tissue that lines the uterus), which typically sheds during menstruation and regrows to support reproduction.
With endometriosis, the endometrial tissue grows excessively, both inside and outside of the uterus, which can cause pelvic pain, extreme menstrual cramping and non-menstrual cramping, as well as chronic fatigue and reduced fertility.
The Government of Canada recently announced funding for endometriosis patients and research, the largest single investment in endometriosis care in Canada for the last 20 years. This much-needed, long-awaited funding will go far to address the many challenges that endometriosis patients face, including struggling to get a diagnosis in the first place, dismissal of their symptoms, related stigma, and ineffective treatments.
Left untreated, endometriosis can affect the central nervous system, leaving patients at heightened risk of abnormal pain and chronic pain presentation, which too often negatively impacts their overall quality of life.
In fact, endometriosis patients often experience a reduced ability to participate in the activities of everyday life. Yolanda Kirkham, an obstetrician-gynecologist (OBGYN) from the University of Toronto, has reported that girls and young women are unable to attend school for a few days each month due to their symptoms, while others with the disease frequently miss work due to nausea and vomiting.
The unfortunate outcome for these patients is not just their reduced ability to participate in activities. It also means they experience significant losses in their economic productivity. Researchers have found that the average endometriosis patient in Canada loses around $3,400 in economic productivity per year.
Delayed diagnosis
One of the significant challenges faced by people with endometriosis is receiving a diagnosis. Patients experience an average delay of 5.4 years from the onset of symptoms to diagnosis. The symptoms are similar to other reproductive health issues (such as polycystic ovary syndrome) or severe period pain, which can be confusing for non-specialist health-care professionals.
Research with endometriosis patients has shown that most cases of endometriosis are not diagnosed by primary care providers, but by specialists—namely OBGYNs to whom they are referred. Taken together with long waiting lists for specialists, the barriers to diagnosis are significant.
Another barrier is that women often have difficulty convincing care providers their pain is real and a cause of concern. In a recent research project, one of us (Sarah Seabrook) examined 70 publicly available accounts of people experiencing endometriosis, including quotes printed in newspapers, as well as from the narratives published by endometriosis not-for-profit EndoAct.
Patients described being dismissed, that their pain was “just muscle pain,” “all women go through this,” and “this is the way cycles are for women,” and to live with it.
This dismissal of pain is particularly troublesome because people don’t often share their menstrual experiences and may be unable to differentiate between normal and abnormal menstrual experiences. In an article published by CBC News in 2021, a woman with endometriosis reported that the first few times she had her period, she was hospitalized for severe pain, but because this was her initial experience of menstruation, “she thought the pain related to her period was normal.”
Lack of effective treatments
Once endometriosis is diagnosed, there are significant barriers to receiving effective treatment. The first line of treatment is typically hormonal birth control, which does nothing to address the growth of endometrial tissue, although for some people it can help with controlling menstrual pain. The same is true of anti-inflammatories and painkillers, which can reduce pain, but do little for the growth of endometrial tissue.
When things are more severe, patients might be given surgical options such as tissue excision (removing the entire endometriosis lesion) or ablation (burning off the surface of the endometriosis lesion). However, these procedures are rarely curative—the excess endometrial tissue grows back in a lot of cases. As a final resort, some patients undergo a hysterectomy. For the most part, endometriosis care is focused on either temporarily reducing pain, or temporarily controlling the growth of tissue.
The lack of effective treatment options is tied to an ongoing failure to understand endometriosis, its underlying causes and effects. Leading Canadian experts have been calling for the improved understanding of endometriosis care and its treatment options, and advocates have been mobilizing for increased funding to understand, diagnose and treat endometriosis in Canada.
To improve outcomes, endometriosis patients need more research, more options and more attention to be paid to the disease. The newly announced federal investment in endometriosis research and care by the federal government is a good first step—although continued funding and support will be needed to address the continued, far-reaching effects of endometriosis in Canada.
Provided by
The Conversation
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Source: Read Full Article
