Measurement of plasma D-dimer levels—a test more commonly used to detect blood-clotting disorders—can provide useful information when making the difficult diagnosis of periprosthetic joint infection (PJI), reports a study in the Journal of Bone and Joint Surgery.
Plasma D-dimer measurement has “comparable diagnostic accuracy” to other commonly used tests for identifying PJI, and in some situations outperforms the standard tests, according to the new research by Javad Parvizi, MD, FRCS, and colleagues of Rothman Orthopaedic Institute at Thomas Jefferson University, Philadelphia.
Can D-dimer help in making the difficult diagnosis of PJI?
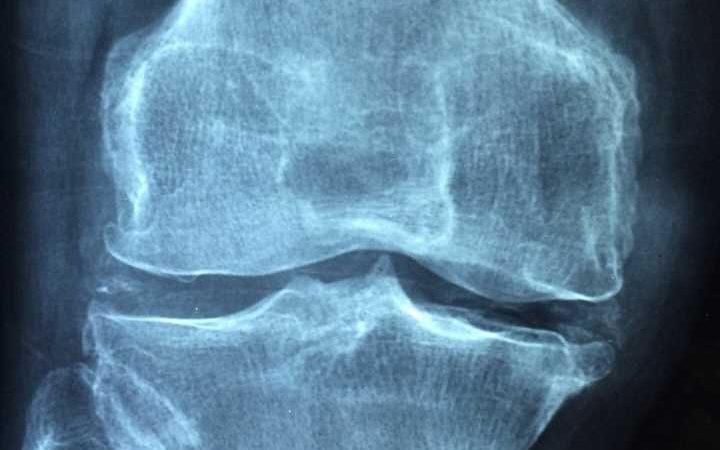
PJI is a devastating complication of failed total hip or knee replacement and is one of the leading causes of implant failure. Diagnosis of PJI can be “extremely challenging,” according to the authors, as no single test has “absolute accuracy” in determining whether or not PJI is present.
Two common markers of inflammation—C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR)—are recommended as screening tests for suspected PJI. However, both have limitations, including a high rate of false-negative results when PJI is present.
Plasma D-dimer is a commonly used test for certain blood clot-related disorders. It is also a potentially useful marker of infection and has been validated for use in the diagnosis of PJI. However, some subsequent studies have raised concerns about the diagnostic performance of D-dimer testing for PJI, and its true accuracy remains unknown.
In the new study, Dr. Parvizi and colleagues compared plasma D-dimer and other tests for the diagnosis of PJI. Over a four-year period, the study prospectively enrolled 502 patients undergoing revision knee or hip arthroplasty regardless of their surgical indication. Immediately before surgery, all patients underwent a blood draw and the levels of D-dimer, CRP, and ESR, and fibrinogen were measured.
After application of the 2018 International Consensus Meeting definition of PJI, 23% of patients were found to have PJI. The four tests had “comparable accuracy” for the diagnosis of PJI. Sensitivity (ability to detect PJI when present) was 81.3% for D-dimer, 90.4% for CRP, 73.9% for ESR, and 74.7% for fibrinogen. On the other hand, specificity (correctly showing that PJI was not present) was 81.7% for D-dimer, 70.0% for CRP, 85.2% for ESR, and 75.4% for fibrinogen. For all four measures, values were higher for patients who were shown to have PJI.
D-dimer found ‘non-inferior’—and sometimes superior—to standard tests for PJI
However, in certain patient subgroups, D-dimer offered a diagnostic advantage. In a subanalysis that excluded patients with certain health conditions associated with inflammation, the D-dimer test outperformed ESR, fibrinogen, and CRP in recognizing the presence of PJI. D-dimer also performed best in detecting PJI caused by slow-growing “indolent” organisms, with higher values for both sensitivity and specificity. In addition, all four tests had better diagnostic performance in patients with suspected PJI in the knee, as compared with PJI in the hip.
The report is the largest prospective study evaluating the performance of different laboratory tests for suspected PJI. The findings support the value of D-dimer testing to make this often-difficult diagnosis. The authors discuss possible limitations of previous studies that questioned the diagnostic value of D-dimer testing.
“We found that plasma D-dimer was noninferior to serum CRP and ESR in the diagnosis of PJI and may be a useful adjunct when screening patients undergoing revision total joint arthroplasty,” Dr. Parvizi and colleagues conclude. The authors highlight the need for further studies and note that no universal diagnostic cutoff point can be determined, due to known variations in D-dimer measurement.
More information:
Saad Tarabichi et al, Plasma D-Dimer Is Noninferior to Serum C-Reactive Protein in the Diagnosis of Periprosthetic Joint Infection, Journal of Bone and Joint Surgery (2023). DOI: 10.2106/JBJS.22.00784
Journal information:
Journal of Bone and Joint Surgery
Source: Read Full Article