Editor’s note: Find the latest COVID-19 news and guidance in Medscape’s Coronavirus Resource Center.
The rapid development of vaccines against Covid-19 has been a triumph of science, with more than half the world’s population inoculated since vaccines first became available in late 2020. But that triumph has not been shared equally around the world, with only 15 percent of people in low-income countries receiving even a single vaccine dose by late March 2022.
One reason for this imbalance is that the mRNA vaccines that have been so successful in wealthy nations are novel, expensive and technologically challenging to produce. Only a few companies have the expertise to manufacture them and high-income countries have hoarded more than 70 percent of doses.
Efforts to ramp up production of mRNA vaccines in middle- and low-income countries are now underway, including in some African countries. But mRNA is fragile and tricky to handle, requiring some vaccines to be stored at ultra-cold temperatures. This adds to the complexity of vaccine manufacture and to the challenges in distribution in remote areas. Vaccines that use genetically modified viruses to introduce coronavirus proteins, like the Johnson & Johnson vaccine, are also relatively new and technically challenging to produce.
A better option is to turn to more traditional vaccine technologies that don’t require as much new infrastructure, says Maria Elena Bottazzi, a vaccine researcher at Baylor College of Medicine in Houston. Bottazzi coauthored a look at Covid-19 vaccines that use more accessible technologies in the 2022 Annual Review of Medicine. Such vaccines deliver whole, inactivated viruses or fragments of viral protein to stimulate the immune system to produce antibodies, and they can be more than 90 percent effective at preventing disease, just like the mRNA vaccines.
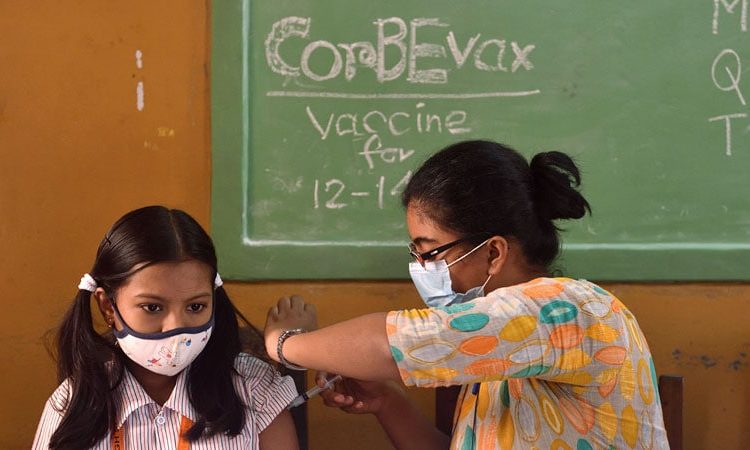
Unlike mRNA technology, factories already exist in many middle- and low-income countries to produce these older types of vaccines, which include the familiar hepatitis A and B and polio vaccines. Such shots also tend to cost less than the new mRNA vaccines: a few dollars a dose, compared to more than $10 per dose. In partnership with the Indian company Biological E, Bottazzi and her Baylor colleague and coauthor Peter Hotez have developed one such Covid-19 vaccine, Corbevax, using protein fragments, which is now licensed for use in India and Botswana.
Knowable Magazine spoke with Bottazzi about what makes a vaccine suitable for global use and some of the barriers that have prevented more widespread vaccination. This conversation has been edited for length and clarity.
What constitutes a “good” vaccine for global use?
You have to have a solid technology that is appropriate for the region, including scalability, storage conditions, the characteristics of the product itself. You have to have the right infrastructure to make, deliver and regulate vaccines. And you have to have all the supplies that are needed to make them. We can’t have sole sources, because then countries block export, as we saw with US-made reagents or India-made vaccines.
Why haven’t mRNA vaccines like those made by Pfizer and Moderna been the solution globally?
We could not make them at large-enough scale. There were not enough production facilities to do this — it was impossible. So even though they did an amazing job scaling to the amount they did, it wasn’t enough. We could not distribute them equally. And of course, then some countries benefited more than others, because there’s the power of purchase. If you can buy them, you hoard the supply.
Is there a better option?
Protein-based vaccines are well suited for becoming a global health vaccine. You have a diversified group of manufacturers that already have all the know-how as well as the prior track record of making them, so they don’t have to start from scratch. And they’re easier to make at large scale, so you have economies of scale.
But I think the most important feature is social. It really depends on the acceptance of these products. A vaccine has to bring confidence to the user. People are afraid — not only because they’re in the middle of a pandemic, but they’re also afraid of all these tools that are new. Some people are clearly early adopters, but there are also many of us who prefer to wait a little bit and see what happens before putting ourselves at risk.
At some level, people are always more confident when they know it’s a vaccine that’s similar to one they’ve been using for many years. That’s why a vaccine such as the one we developed can help. People are more familiar with it because protein-based vaccines are a technology they’ve used before. We get many emails from people asking, “When is your Corbevax vaccine coming to the US? This is the vaccine I’ve been waiting for because I’ve used this kind of vaccine before.” And this is not only happening here, but it’s happening all over the world.
And how you establish clinical safety and efficacy is important. We want to see more inclusion of diverse populations. I think we have that issue now with Covid: Many studies that evaluate the vaccines aren’t done in the populations where these vaccines are eventually going to be used. We need more studies in those countries like Honduras, Ethiopia and Thailand.
Even for familiar vaccine technologies, it takes a lot of work to develop a vaccine for a new disease. You’ve argued that this should be done all around the world, locally or regionally, rather than relying on a few nations. Doesn’t that lead to redundant effort?
You would think that it’s redundant, but Covid clearly showed us that manufacturers and supply chains are too consolidated in very few regions. When you have to address a situation urgently, having those manufacturers concentrated in very few, mostly high-income areas blocks access, and rich countries can hike up the prices or nationalize the vaccines. We are not saying you have to reinvent the wheel everywhere — but strategically, regions have to be able to be self-sufficient so that there can be more equity.
How does your vaccine — which is being developed by an Indian company, Biological E — help achieve this?
We gave BioE the recipe, but ultimately they needed to develop the vaccine themselves. They had to figure out how to make it industrially. They had to become innovators, and now they can teach others to do it, so they can all make their own. That’s very different, because it’s not coming from the traditional multinational model of, “I’m handing it over and you have to do it the way I tell you to.” You’re incentivizing and enabling indigenous production and creativity.
How would you respond to concerns that some countries may lack the technical expertise to produce high-quality vaccines, or the regulatory rigor to evaluate them?
I would totally disagree that these manufacturers, especially middle-income-country manufacturers, are in a lesser category compared to a multinational company. They already produce many vaccines. They have already gone through clinical evaluations by many regulatory agencies. There are quality regulatory agencies in places like Indonesia and India that have been working for years, aligned with international standards. They’ve proven themselves already.
BioE is working for authorization from the World Health Organization. They’re working with the Australian regulatory agency because that’s one of the stringent regulatory agencies that can provide an add-on quality stamp on top of what Indian regulators can give. I think it’s false to say that just because the vaccines are produced in India, they have a different standard than if they were produced in the US or Europe.
Why are Covid vaccines that use the older, more familiar technologies only now becoming available? What made them so much slower to develop?
It’s not slowness. We had a [protein-based vaccine] technology ready three months into the pandemic. And we handed it over to Biological E in May 2020.
BioE struggled to develop it. They did it as fast as they could — it’s just that they certainly did not receive the financial support and they did not receive the governmental support, the political will. Governments said we don’t need you — we’re going to deal with our new technologies, so we’re not going to give you the funding. Now they’re realizing they made a mistake. Now they say, “We want you.”
You’ve made your vaccine technology available to all, patent-free. Should all manufacturers do that?
There are some technologies, like the RNA technologies, which are newer, where there’s a logic why they might want to protect it, because arguably they were developing it for many other therapeutics. They may be more cautious in saying let’s open it up.
We could have patent-protected, but we decided not to. We didn’t want barriers. We basically said, “Look, you want to try our strategy, you can do it by yourself, because it’s all published. But if you want help, we’d be very interested to do co-development with you.”
Covid-19 won’t be the last pandemic. Are there lessons we need to learn for next time?
I think we need to empower countries, especially in the low-middle-income regions — not only with the technology itself, but with regulation, how they create the public health systems. We need to empower them to be more self-sufficient, where they can build a solid workforce and avoid brain drain, but then give them the accountability that they can create their own infrastructure for building that regionally or locally. Not every country has to be self-sufficient for absolutely everything, but they should be complementary to each other. Our vision is of all working together, in the good times and the bad times. But that has to come with political will.
Why should people in wealthier countries care about global vaccine equity? There’s obviously a humanitarian argument — but is there also a practical reason to invest dollars or doses to vaccinate people elsewhere?
We are a big community. Even diseases that primarily affect somewhere else are eventually going to impact us. We see that in Covid. It’s clear that the variants arose from the lack of us ensuring other regions have equitable access to very important tools like vaccines, drugs and diagnostics. Helping others is really helping ourselves.
This article originally appeared in Knowable Magazine on April 18, 2022. Knowable Magazine is an independent journalistic endeavor from Annual Reviews, a nonprofit publisher dedicated to synthesizing and integrating knowledge for the progress of science and the benefit of society. Sign up for Knowable Magazine’s newsletter.
Source: Read Full Article