A new position paper presents an up-to-date review and expert recommendations using the GRADE methodology to inform the implementation of trabecular bone score (TBS) in clinical practice for the management of primary and secondary osteoporosis.
TBS is a gray-level scale textural measurement acquired from dual-energy X-ray absorptiometry lumbar spine images that correlates with bone microarchitecture and which can be used alongside FRAX and bone mineral density measurements to enhance the assessment of fracture risk and to inform treatment initiation and monitoring.
The position paper was authored by an international Expert Working Group appointed by the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the International Osteoporosis Foundation (IOF) under the auspices of the WHO Collaborating Center for Epidemiology of Musculoskeletal Health and Aging (Liège). It encompasses a comprehensive systematic review of 96 high-quality clinical studies from over 20 countries published since 2015, which provide information on the use of TBS for:
- fracture risk prediction in postmenopausal and male osteoporosis
- initiation of treatment and monitoring of treatment effect in postmenopausal osteoporosis
- prediction of fracture risk associated with secondary osteoporosis
- treatment monitoring in secondary osteoporosis
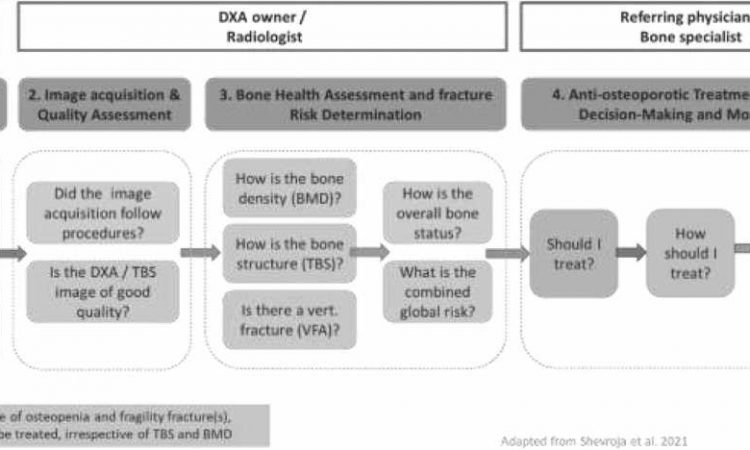
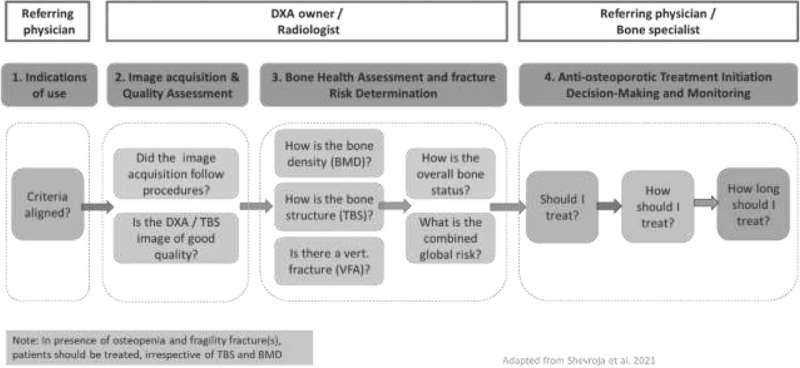
Based on the review, the experts authored 22 statements supporting the role of the TBS software in fracture risk prediction, treatment initiation and monitoring of osteoporosis. The position paper additionally incorporates a more practically focused clinician guide to the incorporation of TBS into clinical pathways for the management of osteoporosis and high fracture risk.
Professor Jean-Yves Reginster, co-author and Director of the WHO Collaborating Center for Epidemiology of Musculoskeletal Health & Aging stated, “Assessing information related to bone microarchitecture in addition to bone density and clinical risk factors provides a more complete assessment to inform management decisions for the benefit of the patient.”
“As there has been considerable new research since the publication of our comprehensive review of TBS in 2015, we judged it was time for a systematic update of the evidence on the clinical use of TBS, via expert consensus to inform practical clinical guidance. As such we have provided a helpful appendix with concise operational guidance that facilitates the integration of TBS in clinical practice, in alignment with clinical workflow.”
Professor Nicholas Harvey, joint-senior author and Chair of the IOF Committee of Scientific Advisors, concluded, “This position paper documents the role of TBS in clinical practice, synthesizing a wide range of evidence across risk assessment, treatment initiation and monitoring, in the context of postmenopausal osteoporosis, osteoporosis in men and secondary causes.”
“The work demonstrates the value of drawing together global expertise to generate what is an evidence-based, but very practical, guide to implementation TBS in the management of osteoporosis and high fracture risk.”
The findings are published in the journal Osteoporosis International.
More information:
Enisa Shevroja et al, Update on the clinical use of trabecular bone score (TBS) in the management of osteoporosis: results of an expert group meeting organized by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO), and the International Osteoporosis Foundation (IOF) under the auspices of WHO Collaborating Center for Epidemiology of Musculoskeletal Health and Aging, Osteoporosis International (2023). DOI: 10.1007/s00198-023-06817-4
Journal information:
Osteoporosis International
Source: Read Full Article