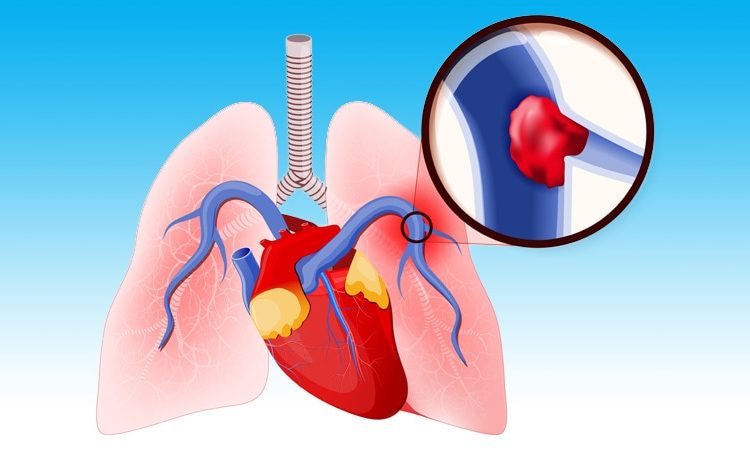
Women with pulmonary embolism (PE) who undergo percutaneous pulmonary artery thrombectomy have higher rates of morbidity and in-hospital mortality than men, a large, nationwide cohort study indicated.
“Female patients hospitalized for PE have been shown to have adverse outcomes when compared to male patients [but] sex-based differences in outcomes for those undergoing advanced interventional therapies such as percutaneous pulmonary artery thrombectomy are currently unknown,” Manyoo Agarwal, MD, David Geffen School of Medicine at the University of California in Los Angeles, and colleagues write.
“Our data suggest that female patients undergoing percutaneous pulmonary artery thrombectomy represent a particularly vulnerable patient population,” they suggest.
The study was published online on August 1 in the journal Chest.
Sample Database
Data were extracted using the Nationwide Inpatient Sample database for the retrospective, cross-sectional study. Among the 1,128,904 patients diagnosed with pulmonary embolism between 2016 and 2018, 0.5% of them underwent percutaneous pulmonary artery thrombectomy. “The primary outcome was in-hospital death,” the authors note.
“When compared with males, females were more likely to belong to > 65-year age group, be African American or Hispanic, and have lower socioeconomic status,” they added. More women, at 16.9%, had procedural bleeding compared with 11.2% of men (P < .05) and required more blood transfusions, at 11.9% vs 5.7% (P < .05). Women also had more vascular complications, at 5%, compared with only 1.5% of men (P < .05).
Importantly, in-hospital mortality rates for women, at 16.9%, were almost double that for men, at 9.3%, with an adjusted odds ratio (aOR) of 1.90 (95% CI, 1.2 – 3.0; P = .003). Among those who survived their hospital stay, women were less likely to be discharged to home, at almost 48%, compared with 60.3% for men, with an aOR of 0.70 (95% CI, 0.05 – 0.99; P = .04), the authors add. Interestingly, length of hospital stay was similar in both groups. As the authors note, the explanation for differences in outcomes between women and men is not clear.
However, as the proportion of patients with PE undergoing catheter-based pulmonary thrombectomy increases, “identifying sex differences in outcomes could potentially help to create sex-specific approaches with respect to patient selection and procedure-related aspects,” the authors suggest. For example, blood transfusion rates might have been higher in women than in men due to lower baseline pre-procedural hemoglobin levels that might lower the threshold for blood transfusion.
“Similarly, sex has been shown to independently predict vascular complications and mortality after vascular access procedures,” the investigators observe. The higher vascular complication rate in women might also be due to their smaller iliofemoral vessels compared with men that could account for the higher risk of complications. “Further studies are needed to validate our findings and to determine the causes of the increased adverse events and healthcare resource utilization that we observed in our cohort of PE patients undergoing percutaneous thrombectomy,” the authors state.
“Efforts can then be directed toward decreasing these events and optimizing healthcare resource use,” they conclude.
Agarwal has reported no relevant financial relationships.
Chest. Published online August 1, 2022. Full text
Follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article