Did the bacteria in your guts when you were a baby impact your risk of future disease? Researchers at Linköping University, Sweden, are aiming to find out. We have talked to two research groups studying whether diseases such as type 1 diabetes and allergy could be prevented by promoting the right bacteria early in life.
Bacteria have been with us throughout human history, and we have evolved together. We swallow and are exposed to various substances that end up in our guts, where an army of immune cells are waiting, ready to defend our bodies.
“You could look at it as mutually assured destruction in our guts. We could get killed if there wasn’t a balance between the permanent bacteria and our immune system which is in direct contact with the gut bacteria. Of course, they learn how to handle each other,” says Johnny Ludvigsson, professor of pediatrics and pediatrician.
So, what is the role of bacteria in maintaining health? One way that researchers have tried to answer this question is by creating mice without gut bacteria. Such studies on animals show that a normal gut flora is hugely important for immune system development and for preventing immuno-related diseases. When it comes to humans, there are still no clear answers to what is cause and what is effect.
The moment a baby is born, bacteria move into the guts. The gut bacteria composition changes a lot in a baby’s first year.
“The gut flora changes as the baby’s diet changes from breast milk or formula to solid food. When babies start crawling and putting things in their mouths, they come into contact with even more things that impact their gut bacteria composition,” says Malin Bélteky, LiU Ph.D. student and medical doctor.
She and her supervisor Johnny Ludvigsson research why some children develop type 1 diabetes when their immune system destroys the cells that produce the hormone insulin. Those affected have to inject insulin for the rest of their lives to regulate blood sugar levels.
“Type 1 diabetes is by far the most life-threatening disease among children and young people in Sweden,” says Johnny Ludvigsson.
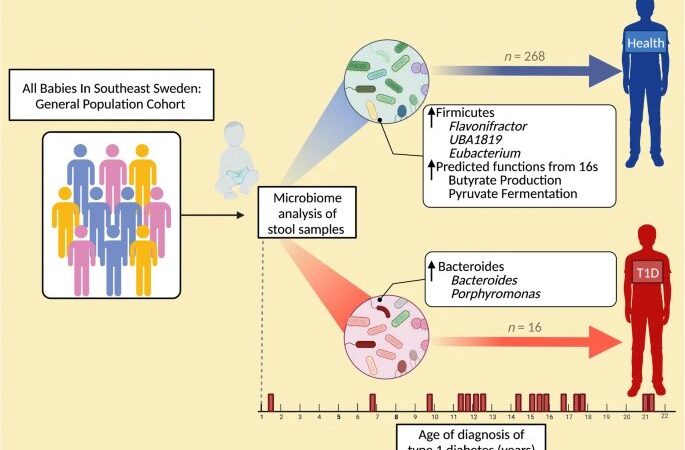
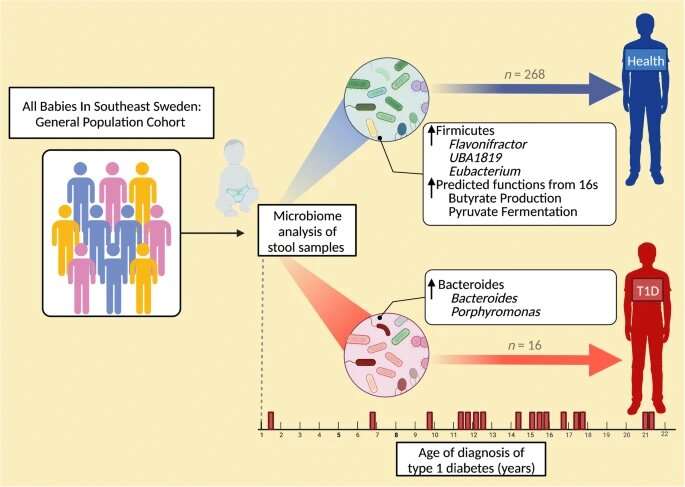
A study recently published in Diabetologia by the LiU researchers and a US research group examined the gut flora of a small group of 1-year-olds who developed type 1 diabetes later in life and compared it with that of children who stayed healthy. The children were matched for maximum similarity in possible impacting factors, such as genetics, breastfeeding and later eating habits.
The study is part of the major ABIS (All Children in Southeastern Sweden) study, where researchers monitor 17,000 children born in the late 90s to investigate the role of gut flora in several autoimmune diseases. It turned out that there were important differences in gut flora composition at age 1 between children who later developed insulin-dependent diabetes and healthy individuals.
“It’s impressive that we can see a link between gut flora at age 1 and something that happens on average 13 years later. This is an indication that our immune system sees dramatic change early in life,” says Johnny Ludvigsson.
“Any attempts to prevent disease from developing must be made very early,” says Malin Bélteky.
Maria Jenmalm, who researches allergic diseases, thinks along the same lines. She and her colleagues were among the first in the world to show differences in gut flora in babies’ first months between those who later developed allergies and those who stayed healthy. This indicates that our early years set the stage for what will happen later. Maria Jenmalm is particularly interested in whether it would even be possible to prevent allergies, by promoting beneficial gut flora as early as possible.
How we are born seems to matter—the gut flora in babies born by Cesarean section differs a lot compared with those born by vaginal birth. Maria Jenmalm’s research has shown that the differences were linked to changes in the babies’ immune response function.
“Nature seems to have solved this by facilitating the transfer of bacteria from mother to baby through vaginal birth,” she says.
A 2016 American study on four children born by Cesarean section involved using a compress to transfer vaginal bacteria from mother to baby. This very small study received much attention, and expectant parents began asking for this treatment.
“Scientific basis on the effects is needed before you start treating many children in this way. You have to weigh risks against benefits, to provide better advice on this much in demand procedure,” says Maria Jenmalm.
She is one of the researchers behind an ongoing Swedish clinical study led from Karolinska Institutet. The question is whether it is possible to counter the impaired supply of bacteria resulting from Caesarian section. In addition to vaginal flora, the study will also involve transferring gut bacteria from mother to baby, to mimic what happens in vaginal birth. Over a two-year period, the study will examine developments in the children’s gut flora and immune system and whether they develop any allergies. It will be a few years’ wait before we know.
But would it be possible to impact the risk of disease even before birth? In another study, Maria Jenmalm and her colleagues are examining the effects of giving pregnant women supposedly beneficial bacterial supplements, known as probiotics, from week 20. The babies are then given the same supplement for a year. The researchers will then monitor the children to see whether the bacteria impact their risk of developing eczema, the type of allergy that occurs at the earliest age.
“The study is still ongoing, so we don’t know yet. But we have noted interesting changes, such as in mothers’ immune responses during pregnancy,” says Maria Jenmalm.
Many huge questions still remain unanswered. What exactly is a “good” gut flora? Could gut flora composition be a direct cause of disease much later? And how much can we ourselves impact our invisible life companions? According to Maria Jenmalm, some of what is said about gut flora in relation to various diseases should be taken with a pinch of salt.
“In some cases, patients may have an inflammation or be under treatment that impacts gut flora. It’s important to be aware that some claims may be exaggerated.”
More information:
Malin Bélteky et al, Infant gut microbiome composition correlated with type 1 diabetes acquisition in the general population: the ABIS study, Diabetologia (2023). DOI: 10.1007/s00125-023-05895-7
Journal information:
Diabetologia
Source: Read Full Article