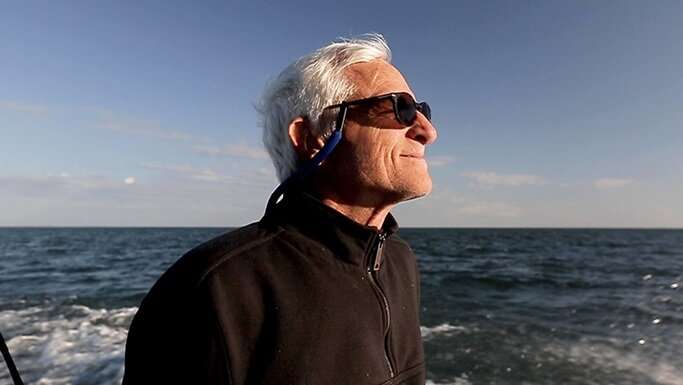
On a chilly day in the fall of 2020, Scott Imbrie’s joyful voice preceded his entrance into the seventh-floor lobby of the Center for Care and Discovery, the University of Chicago Medicine’s flagship hospital located in Hyde Park. He greeted a team of neuroscientists and doctors and dutifully adjusted his face mask before beginning a simple neurological exam.
As Imbrie walked, a distinct sway hinted at why he was there, yet belied what he was once told: that he would never be able to walk or use his arms again.
After his exam, as he settled into a chair and put on a fresh mask—this one covered in the logos of his favorite Chicago sports teams—Imbrie began to share his story.
“I’m doing a lot of things in life that they told me I can never do,” he said. “I broke my neck in 1985, and I was told I was going to be a quadriplegic when I woke up. When they told me that, I knew it wasn’t going to be that way.”
Imbrie was 19 when a car accident damaged his spinal cord and left him paralyzed from the neck down. Though his doctors said it was unlikely, over months of rehabilitation, he relearned how to walk. Now, decades later, he’s pushing the envelope of medical possibility yet again—this time as a subject in a unique research trial that tests the use of neuroprosthetic devices to allow him to sense and manipulate a virtual hand and, eventually, a robotic prosthetic.
In October 2020, Imbrie became the first patient in Chicago and just the fourth person in an ongoing multisite study to undergo the delicate surgical procedure of implanting specialized electrodes into his brain. These electrodes receive neuronal signals from his motor cortex, allowing him to control and manipulate an arm in a virtual reality environment. They also send sensory feedback to his brain, allowing him to experience touch sensations on his hand—so that he can “feel” pressure and vibration.
Ultimately, the UChicago Medicine team plans to connect the system to a robotic prosthetic hand so that Imbrie can use the device in the real world. Refining this research and developing new advanced neuroprosthetic devices will provide new freedom for people who are paralyzed or who are missing a limb.
The study is an expansion of ongoing research conducted at the University of Pittsburgh and UChicago in other paralyzed patients. Like something out of a sci-fi movie, the goal, the researchers say, is to develop technologies that can replace missing limbs or restore touch and movement for those who are paralyzed. Some of the masterminds behind the work include Sliman Bensmaia, Ph.D., an international expert on how the brain encodes and uses sensory information, and Nicholas Hatsopoulos, Ph.D., a leader in the field of the brain basis of motor control and learning.
“The brains of people who are paralyzed can still generate the signals that would normally control movement, but the signal can’t make it past the injury,” said project lead John Downey, Ph.D., a staff scientist at the University of Chicago. “We’re trying to determine how to use that signal from the brain to allow them to control a prosthetic robotic arm and hand. And in addition to being able to control the arm and hand, we want to give them the ability to feel as though their own hand were touching an object when that prosthetic touches an object.”
Making local history
Imbrie’s surgery, conducted on October 27, 2020, was the first time the procedure had been performed in Chicago. Before the surgery could begin, however, the team needed to determine where to put the electrodes. To do this, they had Imbrie undergo a functional MRI scan, which involves recording his brain activity while he imagined moving his hand.
“The surgery is highly complex and involved very precise surgical targeting,” said Peter Warnke, MD, an internationally renowned neurosurgeon at UChicago Medicine. “We used functional MRI to help pin down where these movements are controlled in the brain and used this information to plan the surgery to place hundreds of electrodes in the correct spot. This careful targeting is extremely important because these electrodes needed to be placed in the correct locations for each finger so Scott not only can exert pressure but also feel that sensation as if it were his own hand.”
In fact, the functional MRI allowed for such precise targeting that the researchers were able to place the electrodes that evoke sensations to small patches of skin in Imbrie’s fingers, making it much easier to adjust the robotic hand’s sensory input to align with what a human hand might feel. This is important because, as past research has shown, the brain seems incapable of adjusting the perceived location of a touch even with extended exposure.
Now fully recovered from the procedure, Imbrie makes the trip from his home in Worth, Illinois, over to the UChicago Medicine campus on the South Side of the city three times a week, where he stretches out in a comfortable armchair and waits patiently as graduate students from the Bensmaia and Hatsopoulos labs use long swabs to carefully clean his connectors and scalp before plugging in the device. Looking like something out of “The Matrix,” the two black, rectangular boxes make it easy for the researchers to connect Imbrie to the virtual reality (VR) system he’s been learning to control with his mind.
Using virtual reality
“Manipulating the VR arm is very exciting because when I first started doing it, I tended to try and move my own arm,” said Imbrie. “Now I’ve learned that just thinking about moving it makes it function a lot better. Sometimes when I’m learning to do a new task with the virtual arm and hand, I have to think about how I’d move my real hand and arm just to put it in my mind, so I can imagine doing it with the virtual arm. Sometimes I lose control of the virtual arm, so I hum to myself or close my eyes and rethink how to do it. It’s exciting. There’s a lot of different methods I try to make things work when they’re not working so well.”
During his four-hour-long test sessions, Imbrie performs activities that seem repetitive—with a VR headset slipped over his eyes, he uses his mind to move a floating hand in a virtual reality environment. For this activity, he reaches to pick up a cup from a table, moves it to align with a target presented by the system, and sets it back down. Later, Imbrie will concentrate as the researchers feed his brain sensory information as he reports on where he feels the sensation and what it feels like.
“There are 62 different channels that all affect my sense of touch in a different place,” Imbrie explained. “I feel some of it on the surface in some places, or maybe deep, like underneath the fingernail. And there are distinct differences to the feelings, too—like for the ones that are at the very top of my finger, on the surface, it feels like a paperclip, or a needle pushing on it. But this other one on the edge of my thumb, it feels like when I’m reaching into the evergreens to clean out the needles, and they’re poking at me.”
Even just a few short months after his surgery, Imbrie has progressed rapidly in the study.
“Scott can do a variety of different tasks right now,” said Downey. “He can reach and position the hand in space, grasp and move objects, and even grasp objects with varying amounts of force. He’s also doing sensory tasks, which involve us stimulating his brain and he reports what the sensations feel like, how strong they are, whether they’re tingling or feel like pressure. We’re using this to figure out exactly how we can change the way we stimulate the brain in order to change the sensation Scott feels, and try to make things feel as though his hand were touching a natural object.”
All the data from these repeated trials is then fed into modeling systems that the research team uses to help refine the computer programs that translate Imbrie’s thoughts into movement and provide him with a sense of touch. The hope is to use this information to inform not only future work with Imbrie, but also future studies and—eventually—to develop technologies that can be widely and regularly used by people who are paralyzed or missing limbs.
“All the sensory signals that come from the hand give you information about the objects that you interact with and your interactions with them,” said Bensmaia. “Our goal is to confer to the users of these robots the dexterity with which we are endowed with our own native hands. On the motor side, we want to understand how the brain naturally controls the hand. How can we speak the language of the brain and be able to recognize that language when moving this robotic hand? On the sensory side, when we touch something, how is it that the nervous system responds to that? And how does that neural response give rise to a perceptual experience?”
While the investigators hope to find additional quadriplegic subjects who may be interested in participating in this study, they recognize not all candidates will have the same level of functionality as Imbrie. Imbrie has been an ideal candidate for this trial because of his preexisting spinal cord injury, limited use and sensation of his hands, and willingness to dedicate time to the study—he’s in the lab for 15 hours a week doing experiments.
What’s more, he loves the work.
“Scott is a gift,” Bensmaia said. “He is someone with unbridled enthusiasm, and he is so generous and so positive and so motivated. He came, he had these implants put into his brain, and the next day he was like, “When can we get started?” He has just hit the ground running and is great at everything already.”
Finding the right patients for the future
Later this year, the research team plans to get Imbrie set up with more than just a VR set—they are working to integrate a cutting-edge robotic hand with a robotic arm that Scott will be able to manipulate using the same electrodes that he uses for the VR system. While the technology is far from ready to hit the market, the researchers are thrilled with the work they’ve done with Imbrie so far.
“While the work with Scott is still very early, there are so many potential applications for this research in the future,” said Hatsopoulos. “This could help us develop technology to allow those who are paralyzed or who have lost a limb to do basic daily activities, like dressing or feeding oneself, working on a computer, and even getting up and walking in the form of an exoskeletal robot.”
Imbrie is eager to participate in the project for as long as the electrodes are functional and he is able to help provide more data for the research, even if he won’t benefit directly from the outcomes of the study. For him, he said, it’s more important that the research ultimately can help others.
Source: Read Full Article
