New research presented at this year’s European Congress on Obesity (held online, 10–13 May) reveals an association between increasing body mass index (BMI) and the risk of testing positive SARS-CoV-2, the virus which causes COVID-19. The study is by Dr. Hadar Milloh-Raz, The Chaim Sheba Medical Center, Tel-HaShomer, Ramat-Gan, Israel, and colleagues.
Obesity-related factors, including changes to the innate and adaptive immune systems brought on by excess weight, are believed to be associated with an increased risk of contracting various viral diseases. This association between BMI and viral infection risk suggests that a similar relationship may also exist between an individual’s BMI and their risk of contracting SARS-CoV-2.
This study aimed to assess the relationship between BMI and likelihood testing positive in patients who were tested for SARS-CoV-2 at the largest medical center in the Middle East. The team analyzed the details of patients who had been tested for the virus during a 9-month period, collecting data on BMI, age, sex, and presence of comorbidities including congestive heart failure (CHF), diabetes mellitus (DM), hypertension (HTN), ischemic heart disease (IHD), stroke (CVA), and chronic kidney disease (CKD). The study did not look at COVID-19 mortality or outcomes, only the risk of testing positive.
At the start of the pandemic, the Chaim Sheba Medical Center introduced a policy in which all hospitalized patients were tested for COVID-19, regardless of their symptoms or reason for admission (whether they were suspected to have COVID-19, or for completely different reasons such as elective surgery, traffic accidents). In total 26,030 patients were tested across the study period (between March 16 and December 31, 2020), and 1,178 positive COVID-19 results were recorded. The numbers of patients in each BMI category and the proportion of positive tests varied as shown in the table:
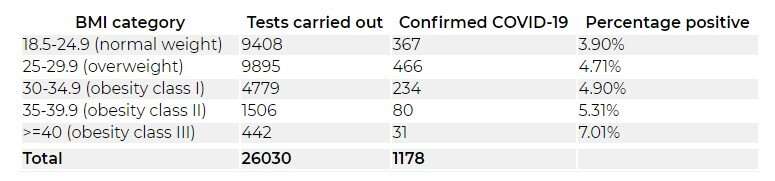
The authors found that the odds of testing positive for SARS-CoV-2 were significantly higher in patients who were overweight or obese compared to those with a normal BMI. Those patients classed as overweight (BMI 25.0-29.9 kg/m2) were 22% more likely to test positive than those of normal weight (BMI 18.5-24.9 kg/m2).
The likelihood of testing positive was even higher in patients with obesity relative to their normal weight counterparts, and those odds rose with increasing BMI. Class I obesity (BMI 30.0-34.9 kg/m2) was linked to a 27% higher risk of testing positive, which increased to 38% for class II obesity (BMI 35.0-39.9 kg/m2), and an 86% higher risk in class III or morbid obesity (BMI at or above 40.0 kg/m2).
The relationship between BMI and the probability of a patient testing positive remained significant even after adjusting for the age and sex of the patient and having accounted for any comorbidities that were present. The authors found that every 1 kg/m2 rise in a patient’s BMI was associated with an increase of around 2% in the risk of testing positive for SARS-CoV-2.
The study also found both positive and negative associations between the risk of testing positive and the presence of comorbidities linked to obesity. Diabetes was associated with a 30% higher likelihood of testing positive, while the risk of testing positive was almost six times greater in patients with hypertension. Conversely, the authors found that the odds of a positive test were 39%, 55%, and 45% lower among patients with a history of stroke, IHD, and CKD, respectively. The authors cannot provide an explanation for why patients with stroke, IHD or CKD would have a lower risk of testing positive for SARS-CoV-2.
Source: Read Full Article
