In a recent study posted to the medRxiv* preprint server, researchers provided quantitative estimates of population-level drivers of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission and infection severity by fitting coronavirus disease 2019 (COVID-19) epidemiological surveillance data from England into dynamic transmission models.
SARS-CoV-2 infections have led to unprecedented morbidity and mortality across the globe, and the continual emergence of SARS-CoV-2 variants has made COVID-19 mitigation challenging. Epidemiological analyses have been performed to assess SARS-CoV-2 variant of concern (VOC) transmissibility and the severity of infections caused by them. However, integrated analyses quantifying the effectiveness of various interventions and directly comparing VOC severity and transmissibility are limited.
 Study: Epidemiological drivers of transmissibility and severity of SARS-CoV-2 in England. Image Credit: Nhemz / Shutterstock
Study: Epidemiological drivers of transmissibility and severity of SARS-CoV-2 in England. Image Credit: Nhemz / Shutterstock
About the study
In the present study, researchers used a dynamic, robust, and validated transmission model and Bayesian inference framework, fitted with comprehensive SARS-CoV-2 surveillance data of individuals residing in England.
Data analyzed included polymerase chain reaction (PCR) reports, population-level COVID-19 prevalence survey data, genomic characterization of PCR-positive COVID-19 cases, seroprevalence data from blood donors’ residual serum samples, hospitalizations, and deaths at the individual level and community level. The relative and absolute transmissibility of SARS-CoV-2 wild-type strains and VOC, such as the Alpha VOC, Delta VOC, and Omicron VOC’s BA.1 sub-VOC were estimated.
The impact of non-pharmaceutical interventions (NPIs), clinical practice changes, care provision changes, immunity induced by previous SARS-CoV-2 infections and vaccinations, and COVID-19 severity was evaluated between 16 March 2020 and 24 February 2022. In addition, the effective reproduction number (Rtff) and the time-varying reproduction number (Rt) in the population lacking anti-SARS-CoV-2 immunity were estimated.
To comparatively assess COVID-19 severity, causative VOC-specific infection hospitalization (IHR), hospital fatality (HFR), and infection fatality ratios (IFR) were determined, and the impact of changes in clinical practices and public immunity levels against COVID-19 severity outcomes was evaluated. In addition, age-stratified COVID-19 severity was assessed, and sensitivity analyses were performed considering transmissibility-affecting variables for all VOCs. For Omicron VOC only, the cross-VOC protection and booster dose vaccine effectiveness (VE) was determined.
Results
Before COVID-19 vaccinations, Rtff was marginally lesser than Rt, indicating low prior infection-induced immune protection, and only stringent levels of NPIs (such as (remote working and face mask use) were effective in curtailing SARS-CoV-2 transmission. The intrinsic transmission advantage of the Alpha VOC and Delta VOC enabled them to gain dominance, and Omicron VOC’s immune-evasiveness and antigenic divergence lowered immunity against SARS-CoV-2 by one-third, allowing Omicron to gain dominance at the end of 2021, despite high levels of public immune protection at the time.
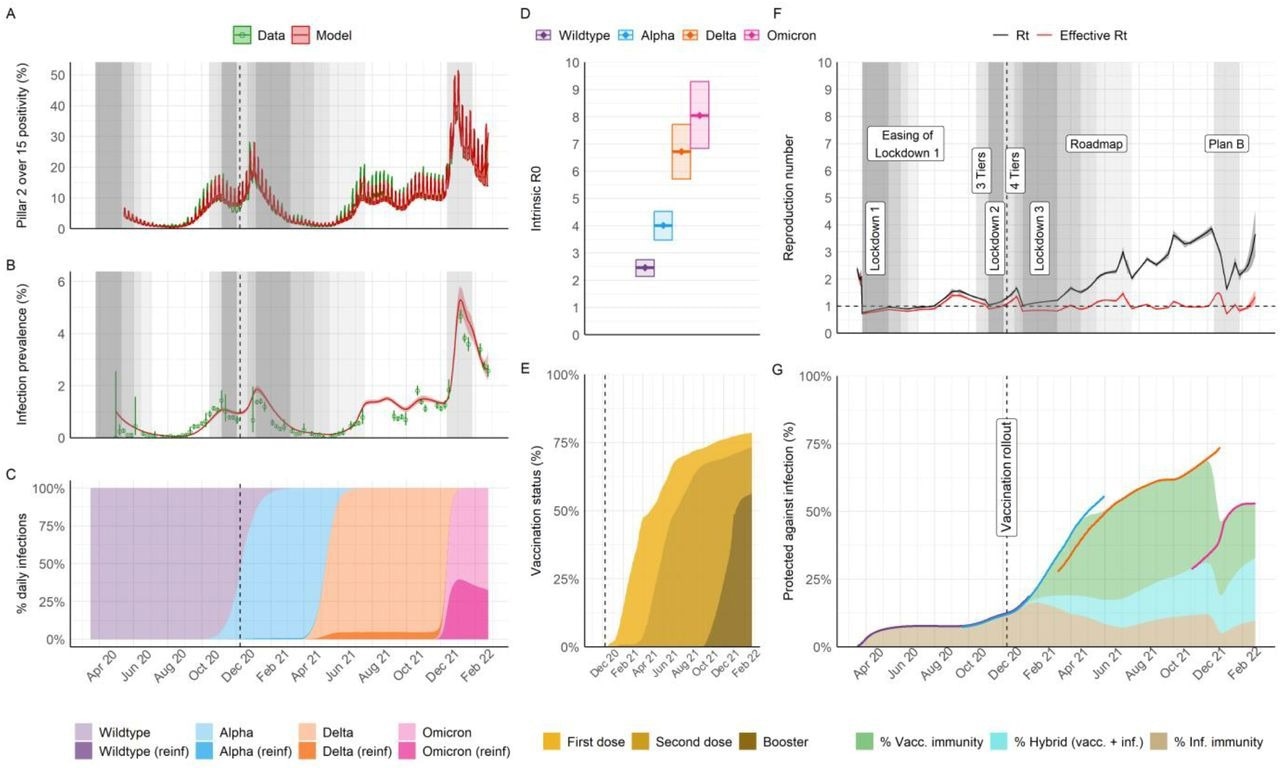
Population-level transmission of SARS-CoV-2 between March 2020 and February 2022 in England. A) Infection positivity measured amongst those aged over 15 years old in the community through the national Government PCR testing program (Pillar 2). B) Infection prevalence (PCR) in representative samples of households from the REACT-1 study. In A and B, data is shown in green (lines and points, with binomial 95% confidence intervals in error bars) and model trajectory in red (average and 95% credible interval (95% CrI)). Grey shading indicates periods where specific non-pharmaceutical interventions (NPIs) of interest for the analysis were implemented nationally; see legends in panel F and the main manuscript for specific references. The shading level is not correlated with quantitative astringency; for a complete list of modeled change points in contact rates including dates and description see Supplement Table S11 and Figures S28 and S29. C) Model-inferred average frequency of daily infections by variant and type of infection (either primary or re-infection following any prior infection, “reinf”). D) Intrinsic R0 estimates by variant (mean and 95% CrI). E) Model trajectory of vaccine status of the national population (all ages as the denominator), as informed by official data of daily doses administered (see sources in Table S1). F) Model trajectories of the instantaneous reproduction number in the absence of the effect of immunity (Rt) or accounting for immunity (effective Rt). Legends and grey areas specify the date and duration of official NPIs in England over the study period. G) Inferred effective levels of protection in the population (all ages as the denominator. Lines correspond to the effective protection against specific variants, with the color scheme as in panels C & D, whereas areas indicate overall effective protection by type of immunity (vaccine-derived, hybrid, or natural from prior infection). During periods of variant replacement (e.g. Alpha to Delta) the effective protection transitions from the levels associated with the variant being replaced to the level of the variant that becomes dominant.
Immunology eBook
The Alpha VOC exhibited the greatest basic IFR and HFR, followed by the Delta VOC, the wild-type strain, and the Omicron BA.1 VOC. The Omicron BA.1 sub-VOC showed basic severity properties similar to the wild-type strain IHR, HFR, and IFR. NPIs were gradually lifted during the Delta wave, and the Delta VOC carried a significantly elevated risk of hospitalization and death. The findings indicated that the re-adaptation of hospital capacities and swift development of effective therapies (such as dexamethasone and remdesivir) would effectively combat wild-type strain infection severity. Clinical care improvements could be nullified if not coupled with timely and effective and timely interventions for COVID-19 mitigation.
Transmissibility increased with every successive VOC, and BA.1 had the highest basic reproduction number at 8.1. In contrast to previous studies, Alpha VOC had the greatest basic IFR (2.8%), followed by Delta (2.0%), wild-type (1.2%), and Omicron (0.6%). The basic IHRs for the wild-type strain, Alpha VOC, Delta VOC, and Omicron VOC, were 2.20%, 3.50%, 4.40%, and 3.50%, respectively. The HFRs for the corresponding strains were 33%, 48%, 30%, and 11%, respectively. Spike (S) protein mutations in Alpha and Delta VOCs conferred more significant angiotensin-converting enzyme 2 (ACE2) receptor binding affinity and enabled swifter fusion with host cell membranes.
The R0 values for the wild-type strain, Alpha, Delta, and Omicron BA.1 VOCs were 2.5, 4.0, 6.7, and 8.1, respectively. Only 8.0% of the general public was immune by the beginning of September 2020, before Alpha VOC’s emergence. Population-level immunity increased rapidly from 12.0%, from prior COVID-19 only, on 8 December 2020, to 34.0%, during Delta VOC emergence in March of 2021, resulting from hybrid immunity. A peak in population immunity was estimated at 68.0% at the end of November 2021, mainly due to vaccinations. Sensitivity analyses yielded similar results as the primary analysis.
NPIs were not timely enough or always effective in controlling SARS-CoV-2 transmission, leading to peaks in hospitalization rates during the winter of 2020 and 2021, with elevations in HFR that could not be explained only by the wild-type strain or Alpha VOC severity characteristics or changes in the age groups of hospital admissions. In addition, immune protection from prior infections has been consistently low in England, and risk-prioritized vaccinations could lower VOC transmission and severity.
The combined fraction of individuals protected effectively against SARS-CoV-2 by prior infections and by hybrid immunity (induced by infections and vaccinations), was estimated to be 23%. Failure to curtail SARS-CoV-2 spread early could enhance COVID-19 severity and strain on healthcare services, and boosting immunity by vaccinations could reduce the global burden of COVID-19.
Overall, the study findings highlighted the population health implications of greater VOC transmissibility, resulting in greater virulence and immune evasiveness. Despite comparable severity as Omicron, VOCs with greater transmissibility would significantly threaten global health. The study findings provided valuable insights into the driving factors of COVID-19 dynamics, could inform future intervention development, and indicated that optimized surveillance efforts to identify changes in VOC transmissibility, infections, and severity and novel VOC emergence are essential.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Epidemiological drivers of transmissibility and severity of SARS-CoV-2 in England. Pablo N Perez-Guzman et al. medRxiv preprint 2023, DOI: https://doi.org/10.1101/2023.02.10.23285516, https://www.medrxiv.org/content/10.1101/2023.02.10.23285516v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, binding affinity, Blood, Cell, Coronavirus, Coronavirus Disease COVID-19, Dexamethasone, Enzyme, Frequency, Genomic, Global Health, Healthcare, Hospital, immunity, Mortality, Omicron, Polymerase, Polymerase Chain Reaction, Protein, Receptor, Remdesivir, Reproduction, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Vaccine

Written by
Pooja Toshniwal Paharia
Dr. based clinical-radiological diagnosis and management of oral lesions and conditions and associated maxillofacial disorders.
Source: Read Full Article