Liza Makowski, Ph.D., professor in the Department of Medicine and the UTHSC Center for Cancer Research, has long been interested in how the immune system is altered by obesity and how this impacts cancer risk and treatment.
“Obesity is complex, because it can cause both inflammation and activate counter-inflammation pathways leading to immunosuppression,” Dr. Makowski said. “How obesity impacts cancer treatments is understudied.”
Obese patients with breast cancer often have worse outcomes than non-obese patients. However, exciting developments are being made in other cancers that may also hold promise for treating breast cancer. In studies of a new type of immunotherapy drug, called a checkpoint inhibitor, obese patients appear to respond better, compared with their leaner counterparts in some cancers, such as melanoma, ovarian, certain lung, and kidney cancers. It is not clear if this finding is also true for breast cancer patients.
Dr. Makowski teamed up with Joe Pierre, Ph.D., assistant professor in Pediatrics and director of the UTHSC Center for Gnotobiotics, to investigate how obesity impacts immunotherapy and to identify potential biomarkers of success.
New findings they published in the June issue of Cell Reports have provided some clues to how breast cancer patients might respond.
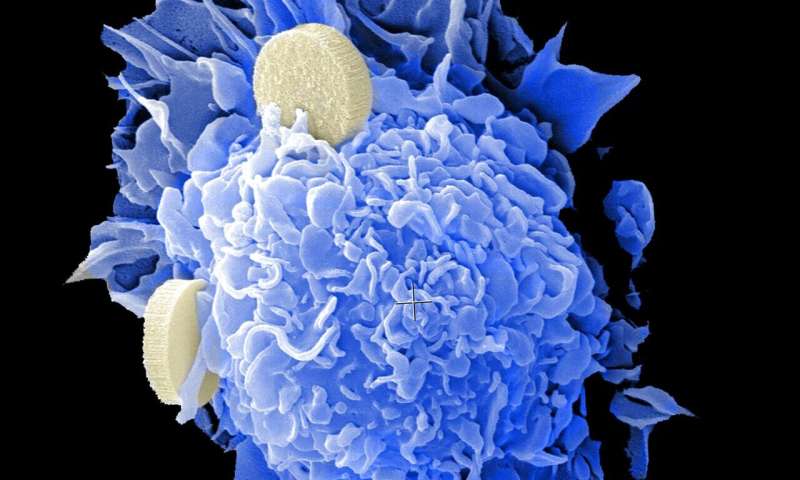
Immunotherapies, such as immune checkpoint inhibitors, including atezolizumab (TECENTRIQTM, anti-PD-L1) or Pembrolizumab (KeytrudaTM, anti-PD-1), have been approved in 2019 and 2020, respectively, to treat some patients with triple negative breast cancer, a highly aggressive subtype. It is not currently known if obese breast cancer patients respond better to immunotherapies, similar to findings reported with melanoma. Clinical studies such as these are eagerly awaited by breast cancer patients and researchers.
Drs. Makowski and Pierre showed that obesity in mouse models led to accelerated tumor growth, compared to lean counterparts. Anti-PD-1 immune checkpoint blockade successfully blocked obesity-driven cancer progression. Anti-PD-1 increased immune cell numbers and effective anti-tumor markers. By comparing mice that didn’t have tumors to mice with tumors, the team showed that the presence of the tumor exacerbated an environment allowing tumors to hide, resulting in high levels of immunosuppressive cells that were ineffective to reduce breast cancer.
Fortunately, these ‘sleepy cells’ could be reprogrammed to reinvigorate anti-tumor immunity with anti-PD-1, despite persistent obesity. The group also worked to identify changes in the gut microbiome associated with obesity and a strong response to therapy.
The Makowski and Pierre labs are currently funded by the National Cancer Institute to further investigate why certain microbes may impact cancer therapies.
Source: Read Full Article
