Researchers have developed an animal model to test HIV infection and therapies in infants, allowing them to develop biomarkers to predict viral rebound after antiretroviral therapy (ART) interruption. The simian-human immunodeficiency virus (SHIV)-infected infant rhesus macaque model, a collaborative effort among researchers at several institutions, is described in a recent issue of the journal mBio.
“To date, all of the animal models that have been developed for studying novel therapies in nonhuman primate models around HIV have been in adult animals. A lot of those are immune based strategies, and we know that infants have a developing immune system that has distinct qualities,” said study principal investigator Sallie Permar, MD, PHD, professor of pediatrics in the Division of Infectious Diseases; professor of molecular genetics and microbiology, immunology, and pathology; and member of Duke Human Vaccine Institute. “It is important to develop a model by which we can study infected infants and study the interventions that can be implemented to reduce the viral reservoir and delay time to rebound after stopping antiretroviral therapy.”
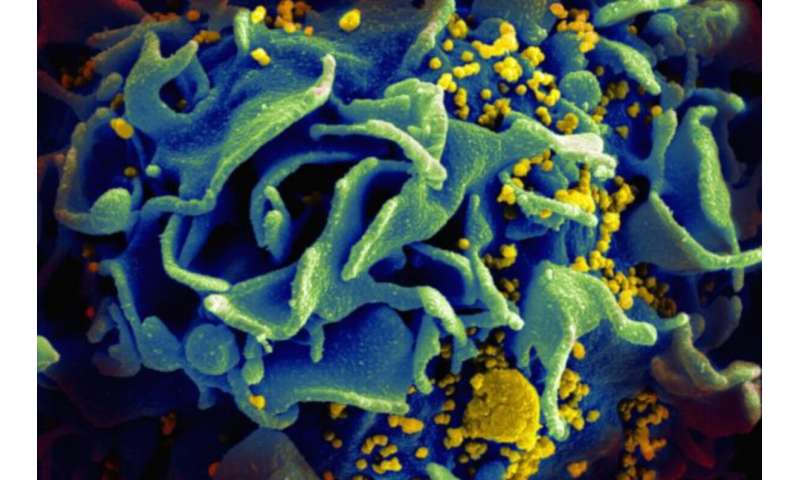
The new model allows for immune interventions against the HIV envelope protein through the use of a SHIV, as opposed to a SIV, a simian immunodeficiency virus that has a very different virus envelope than HIV. Differences exist in the infant modes of HIV acquisition and immune responses, compared with adults or adolescents who become infected mostly through the sexual route. Moreover, this model takes advantage of recent advances in SHIV development that fully replicated the clade C viruses that are involved in the majority of infant HIV transmission. Researchers at the University of Pennsylvania have developed a new way to make SHIV, in which mutations are made around the CD4 binding site that HIV uses for entry into cells.”This opened up a new treasure trove of SHIVs that would be available for this type of model,” said Dr. Permar.
In the study, the researchers infected the infant monkeys with the new SHIV in the first one to two months of life, simulating a breast milk transmission. They then started the animals on antiretroviral therapy 12 weeks later and stopped treatment after a few months.They evaluated plasma virus load and found that the virus reached high peak virus load and responded quickly to therapy, which simulates what is seen in human infants.
The researchers then compared the viral replication kinetics and reservoir in infant rhesus macaques to that seen in a separate study of adult rhesus monkeys infected with the same SHIV strain. Infant monkeys had their virus rebound a couple of weeks after stopping the drugs, which was similar to adults, but adults had better virus control after rebound. “There are going to be differences in the infant and adult based therapies that are aimed at extending the time to viral rebound after stopping antiretroviral therapies,” said the lead author of the study Ria Goswami, PHD, a postdoctoral associate at the Duke Human Vaccine Institute. “Novel interventions that do not rely on daily adherence to antiretroviral therapy are needed to achieve sustained viral remission for perinatally infected children, who currently rely on lifelong ART.”
The researchers are already at work using the new model to test novel immune-based therapies, including monoclonal antibody therapies directed against the HIV envelope, to extend the time to virus rebound after stopping therapies. “A few years ago, a Mississippi baby who went on treatment quickly after delivery and exposure to HIV, and was then taken off therapy unintentionally, had no detectable virus for over two years. Eventually, the virus did return,” said Dr. Permar.”We are interested in how we can make it more likely to have more children like that.”
Source: Read Full Article
