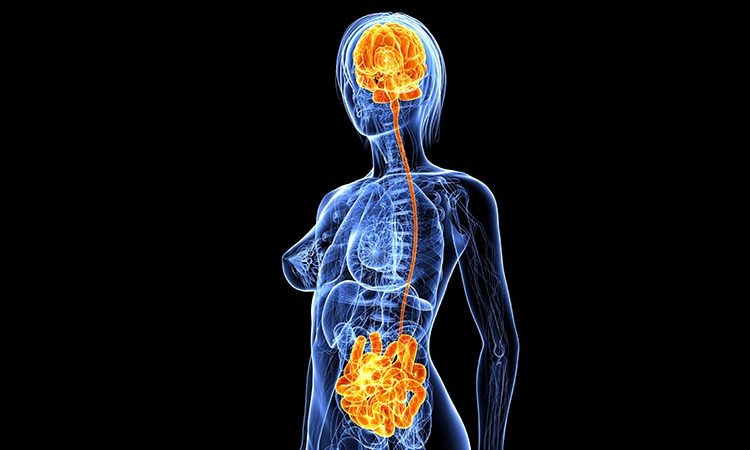
Major depressive disorder (MDD) is linked to disruptions in energy and lipid metabolism, possibly caused by the interplay of the gut microbiome and blood metabolome, new research suggests.
Investigators found that MDD had specific metabolic “signatures” consisting of 124 metabolites that spanned energy and lipid pathways, with some involving the tricarboxylic acid cycle in particular. These changes in metabolites were consistent with differences in composition of several gut microbiota.
The researchers found that fatty acids and intermediate and very large lipoproteins changed in association with the depressive disease process. However, high-density lipoproteins and metabolites in the tricarboxylic acid cycle did not.
“As we wait to establish causal influences through clinical trials, clinicians should advise patients suffering from mood disorders to modify their diet by increasing the intake of fresh fruits, vegetables, and whole grains, as these provide the required fuel/fiber to the gut microbiota for their enrichment, and more short-chain fatty acids are produced for the optimal functioning of the body,” study investigator Najaf Amin, PhD, DSc, senior researcher, Nuffield Department of Population Health, Oxford University, United Kingdom, told Medscape Medical News.
“At the same time, patients should be advised to minimize the intake of sugars and processed foods, which are known to have an inverse impact on the gut microbiome and are associated with higher inflammation,” she said.
The study was published online April 19 in JAMA Psychiatry.
MDD Poorly Understood
Although most antidepressants target the monoamine pathway, “evidence is increasing for a more complex interplay of multiple pathways involving a wide range of metabolic alterations spanning energy and lipid metabolism,” the authors write.
Previous research using the Nightingale proton nuclear magnetic resonance (NMR) metabolomics platform showed a “shift” toward decreased levels of high-density lipoproteins (HDLs) and increased levels of very low-density lipoproteins (VLDLs) and triglycerides among patients with depression.
The gut microbiome, which is primarily modulated by diet, “has been shown to be a major determinant of circulating lipids, specifically triglycerides and HDLs, and to regulate mitochondrial function,” the investigators note. Patients with MDD are known to have disruptions in the gut microbiome.
The gut microbiome may “explain part of the shift in VLDL and HDL levels observed in patients with depression and if the metabolic signatures of the disease based on Nightingale metabolites can be used as a tool to infer the association between gut microbiome and depression.”
Amin called depression “one of the most poorly understood diseases, as underlying mechanisms remain elusive.”
Large-scale genetic studies “have shown that the contribution of genetics to depression is modest,” she continued. On the other hand, initial animal studies suggest the gut microbiome “may potentially have a causal influence on depression.”
Several studies have evaluated the influence of gut microbiome on depression, “but, due to small sample sizes and inadequate control for confounding factors, most of their findings were not reproducible.”
Harnessing the power of the UK Biobank, the investigators studied 58,257 individuals who were between the ages of 37 and 73 years at recruitment. They used data on NMR spectroscopy–based plasma metabolites in depression. Individuals who didn’t report depression at baseline served as controls.
Logistic regression analysis was used to test the association of metabolite levels with depression in four models, each with an increasing number of covariates.
To identify patterns of correlation in the “metabolic signatures of MDD and the human gut biome,” they regressed the metabolic signatures of MDD on the metabolic signatures of the gut microbiota and then regressed the metabolic signature of gut microbiota on the metabolic signatures of MDD.
Bidirectional 2-sample Mendelian randomization was used to ascertain the direction of the association observed between metabolites and MDD.
Individuals with lifetime and recurrent MDD were compared with controls (6811 vs 51,446 and 4370 vs 62,508, respectively).
Participants with lifetime MDD were significantly younger (median [IQR] age, 56 [49–62] years vs 58 [51–64] years) and were more likely to be female in comparison with controls (54% vs 35%).
“Novel Findings”
In the fully adjusted analysis, metabolic signatures of MDD were found to consist of 124 metabolites that spanned energy and lipid metabolism pathways.
The investigators note that these “novel findings” included 49 metabolites encompassing those involved in the tricarboxylic acid cycle ― citrate and pyruvate.
The findings revealed that fatty acids and intermediate and VLDL changed in association with the disease process. On the other hand, HDL and the metabolites in the tricarboxylic acid cycle did not.
“We observed that the genera Sellimonas, Eggerthella, Hungatella, and Lachnoclostridium were more abundant, while genera Ruminococcaceae…, Coprococcus, Lachnospiraceae…, Eubacterium ventriosum, Subdoligranulum, and family Ruminococcaceae were depleted in the guts of individuals with more symptoms of depression,” said Amin. “Of these, genus Eggerthella showed statistical evidence of being involved in the causal pathway.”
These microbes involved are involved in the synthesis of important neurotransmitters, such as gamma aminobutyric acid, butyrate, glutamate, and serotonin, she noted.
Butyrate produced by the gut can cross the blood-brain barrier, enter the brain, and affect transcriptional and translational activity or be used by the cells for generating energy, she added. “So basically, butyrate can influence depression through several routes — ie, via immune regulation, genomic transcript/translation, and/or affecting energy metabolism.”
No Causality
Commenting on the study for Medscape Medical News, Emeran Mayer, MD, distinguished research professor of medicine, G. Oppenheimer Center for Neurobiology of Stress and Resilience and UCLA Brain Gut Microbiome Center, called it the “largest, most comprehensive and best validated association study to date providing further evidence for an association between gut microbial taxa, previously identified in patients with MDD, blood metabolites (generated by host and by microbes) and questionnaire data.”
However, “despite its strengths, the study does not allow [us] to identify a causal role of the microbiome alterations in the observed microbial and metabolic changes (fatty acids, Krebs cycle components),” cautioned Mayer, who was not involved with the study.
Moreover, “causality of gut microbial changes on the behavioral phenotype of depression cannot been inferred,” he concluded.
Metabolomics data were provided by the Alzheimer’s Disease Metabolomics Consortium. The study was funded wholly or in part by grants from the National Institute on Aging and Foundation for the National Institutes of Health. It was further supported by a grant from ZonMW Memorabel. Amin reports no relevant financial relationships. The other authors’ disclosures are listed on the original article. Mayer is a scientific advisory board member of Danone, Axial Therapeutics, Viome, Amare, Mahana Therapeutics, Pendulum, Bloom Biosciences, APC Microbiome Ireland.
JAMA Psychiatry. Published online April 19, 2023. Abstract
Batya Swift Yasgur, MA, LSW is a freelance writer with a counseling practice in Teaneck, New Jersey. She is a regular contributor to numerous medical publications, including Medscape and WebMD, and is the author of several consumer-oriented health books as well as Behind the Burqa: Our Lives in Afghanistan and How We Escaped to Freedom(the memoir of two brave Afghan sisters who told her their story).
For more Medscape Psychiatry news, join us on Facebook and Twitter.
Source: Read Full Article