Despite improvements in access to health coverage under the Affordable Care Act (ACA), racial disparities in breast cancer mortality rates persist and the underuse of advanced breast imaging may be one culprit, experts say.
In a recent position statement, researchers highlighted the disproportionally high breast cancer mortality rates among Black women in Louisiana — a state that has one of the highest breast cancer mortality rates in the nation. In 2019, the breast cancer mortality rate among Black women in Louisiana was 29.3 per 100,000 women compared with the national rate of 19.4 per 100,000.
Although Louisiana has made strides in improving access to breast cancer screening in recent years, the use of advanced imaging — specifically breast MRI — remains underused in this high-risk population. A major barrier to wider use of breast MRI has been cost, and ACA expansion led to higher, not lower, out-of-pocket costs for this screening modality.
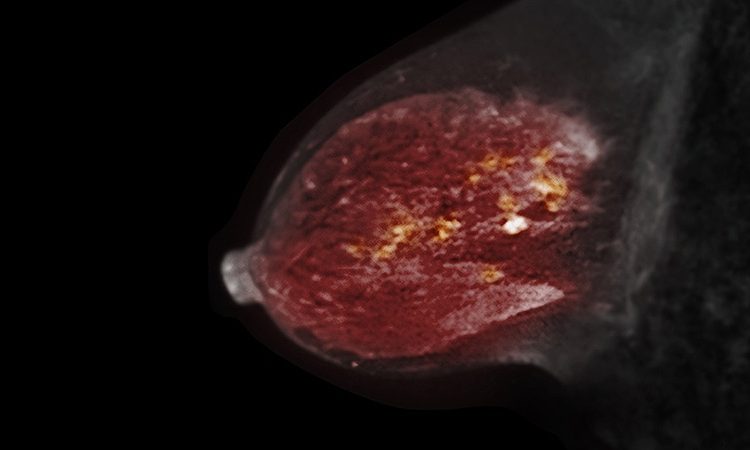
“Breast MRI is a powerful imaging tool for early detection and for screening women at high risk for breast cancer,” the researchers, led by Brooke L. Morrell, MD, of Louisiana State University Health and Sciences Center, write.
However, greater access to healthcare has not necessarily translated to increased breast MRI screening or improved survival among Black women. Even years after the adoption of the ACA, “Black women in Louisiana continue to die of breast cancer at rates significantly greater than the national average,” the authors write.
The position statement was published earlier this month in Cancer.
Breast MRI is known to provide the highest rate of breast cancer detection among commonly used imaging options, with a sensitivity ranging from 81%–100%. That’s about twice as high as the sensitivity range for mammography after factoring in breast density.
“This is of particular importance when we consider the risk‐based screening of younger populations, in which dense breasts are more prevalent,” the authors explain.
For Black women in particular, studies show nearly a quarter (23%) who develop breast cancer are diagnosed under the age of 50 compared with 16% of White women. Black women are also more likely to develop more aggressive, premenopausal breast cancers, including triple-negative breast cancer, that are more easily detected on MRI.
“Adding supplemental screening breast MRI to annual mammography in higher risk women has been shown to detect up to 18 additional cancers out of 1000 patients,” Morrell said. And “many of these cancers are detected much earlier than with mammography alone.”
Still, with ACA expansion, out-of-pocket costs for breast MRI actually increased. This increase likely occurred, in part, because the financial protections outlined in the ACA’s Women’s Preventive Services Guidelines covered mammograms but not breast MRI.
More specifically, under the ACA, Medicaid and most private health insurance plans are required to provide coverage for mammograms at no cost to the patient. The percentage of health plans providing zero cost-sharing for mammograms increased under the ACA from 81.9% to 96.8%, but the corresponding rates of zero-cost sharing for breast MRI screening went in the opposite direction — from 43.1% in 2009 to only 26.2% in 2017, a 2022 study found.
This study also highlighted geographic variations in zero cost‐sharing and out-of-pocket costs for screening breast MRI, with a higher financial burden observed for women living in the South. In addition, studies have demonstrated that race and socioeconomic factors, including education and income, play a role in the underuse of screening, including breast MRI.
These factors all likely contribute to screening breast MRI remaining inaccessible to many women, Morrell and colleagues said.
The authors also outlined three key action items that could help address barriers to MRI breast screening, which include:
-
Reducing the high cost of breast MRI
-
Lobbying to include breast MRI in ACA protections
-
Addressing knowledge gaps among patients and clinicians to better identify women who might benefit from breast MRI
On the financial front, the team explained that a central driver for high costs is the scan time for breast MRI, which could be substantially reduced from 30 to 5 minutes, using an abbreviated protocol.
“Widespread use of low‐cost breast abbreviated MRI screening could remove the cost barrier of adding breast MRI screening to ACA coverage,” without compromising diagnostic accuracy, the authors note.
Further efforts should focus on overcoming cultural barriers, including fear and mistrust of the healthcare system among Black women. Outreach efforts could include public campaigns or town hall and church gatherings that enlist patient navigators, advocates, or community members.
“Our visibility in the community builds trust and affords us the opportunity to share knowledge that may empower women to be their own health advocates,” the authors write.
In terms of the feasibility of revising ACA policies to improve breast MRI access and affordability, Morrell pointed to improvements made in colon cancer screening.
“Studies have demonstrated that after ACA policy changes lowering out-of-pocket cost for colonoscopies, screening colonoscopy rates significantly increased among men, predominantly in socioeconomically disadvantaged population,” she noted. “Similarly, we should investigate how to this can be applied to screening breast MRI.”
Cancer. Published online January 12, 2023. Abstract
For more from Medscape Oncology, join us on Twitter and Facebook
Source: Read Full Article