Severe acute respiratory syndrome coronavirus 1 (SARS-CoV-1) 1 and the novel SARS-CoV-2 coronaviruses enter host cells via angiotensin-converting enzyme 2 (ACE2) receptors. ACE2 receptors are highly expressed in lung alveolar epithelial cells, enterocytes of the small intestine, and arterial and venous endothelium. Previous studies have associated high levels of plasma ACE2 with an increased risk of severe illness from SARS-CoV-2 infection, progressing to coronavirus disease 2019 (COVID-19).
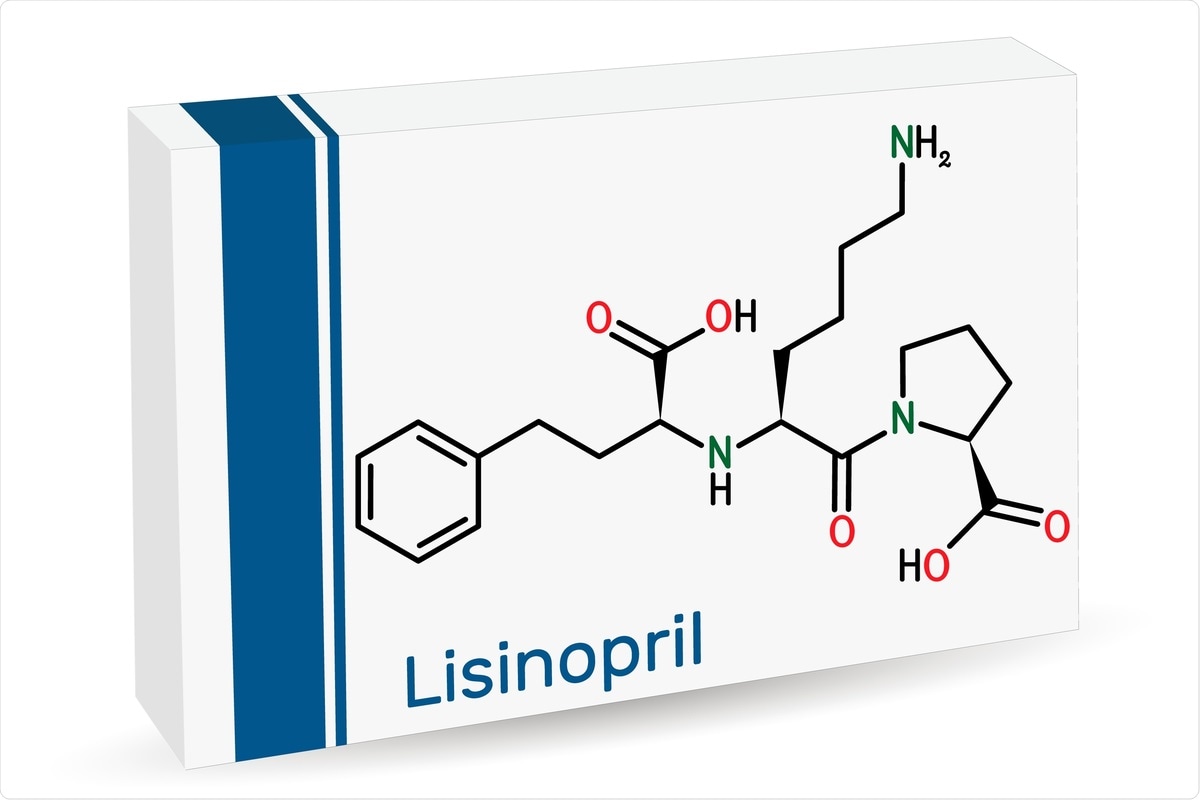 Study: Oral Lisinopril Raises Tissue Levels of ACE2, the SARS-CoV-2 Receptor, in Healthy Male and Female Mice. Image Credit: Bacsica/ Shutterstock
Study: Oral Lisinopril Raises Tissue Levels of ACE2, the SARS-CoV-2 Receptor, in Healthy Male and Female Mice. Image Credit: Bacsica/ Shutterstock
Due to the vital role of ACE2 in viral pathogenesis and the widespread abundance of ACE2 in tissues, scientists speculated if ACE inhibitors and/or angiotensin receptor blockers (ARB) may alter ACE2 tissue abundance and thereby change the host susceptibility to infection with SARS-CoV-2 or the progression, severity, and tissue-specific pathology of COVID-19. The following study is undertaken in mice models by researchers from the National Institutes of Allergy and Infectious Diseases.
Aim of the study
A new study, published in the preprint server bioRxiv*, aimed to determine whether ACE2 targeting drugs change the tissue levels of ACE2 in healthy mice. The researchers investigated the role of ACE1 inhibitors (e.g., lisinopril) or angiotensin receptor blockers (e.g., losartan), as monotherapies or in combination, in altering the ACE2 tissue expression.
They found that oral lisinopril increased ACE1 in tissue relevant to the SARS-CoV-2 transmission and pathogenesis of COVID-19. This was not observed when lisinopril was administered in combination with oral losartan.
The researchers performed a tissue-specific (lung, small intestines, kidney, and brain) study, and variation of tissue ACE2 between tissues, plasma ACE2 correlation with tissue ACE2, and difference of tissue ACE2 levels between male and female mice.
Despite a lack of clinical studies identifying a clear relationship between ACE inhibitor use or ARB use and disease risk or severity in COVID-19 patients, current guidelines support the continuance of ACE inhibitors or ARB during infection. The present study provides preclinical data on how ACE inhibitors and ARB change tissue abundance of ACE2.
About the study
To observe the effect of ACE inhibtor/ARBs, the researchers measured tissue-specific changes in ACE2 abundance following treatment with an ACE inhibitor (lisinopril), an ARB (losartan), or the combination of both, compared to the vehicle, in mice.
The study comprised five female and five male eight-week-old C57Bl/6J mice in each drug treatment group: lisinopril, losartan, lisinopril, and losartan combined, or vehicle control. The mice were treated with the drugs in drinking water for 21 days. The vehicle control was standard drinking water alone. To achieve a 10mg/kg/day drug dosage in the daily drinking water, the researchers initially estimated the mice's average daily drinking water intake. Based on this, they adjusted the drug concentration weekly to maintain consistent dosing throughout the study.
While half the mice were euthanized for collection of plasma and tissues, the other half were transitioned to drinking water for another 21 days to test if the drug-induced changes in ACE2 resolved after drug cessation.
From the flash-frozen tissue samples, the researchers measured the total protein concentration using the BCA assay and the ACE2 tissue abundance by ELISA. They calculated the ACE2 protein index by dividing the ELISA-measured concentration by the total protein concentration of each specimen.
They found that the lisinopril treatment raised the ACE2 protein index in tissues. However, the combination of lisinopril and losartan did not raise tissue levels of ACE2. In the tissue-specific profiling of the ACE2 abundance, the researchers found it was highest in the small intestine, followed by kidney, lung, and brain.
The researchers examined the gene expression in small intestine, which was the tissue with the highest ACE2 protein index. They found that only the lisinopril/losartan combination treatment suppressed ACE2 gene expression in the small intestine. Lisinopril and losartan monotherapy did not change the ACE2 expression.
Concerns of fecal-oral transmission suggest that the intestinal tract may be a site of viral transmission – this needs to be investigated further among people taking ACE inhibitors as the associated increases in small intestine ACE2 could potentially increase the risk of SARS-CoV-2 viral infection.
Even after discontinuation of the drug up to 21 days, the researchers found the drug-induced elevation of ACE2 protein index persisted. To identify whether plasma ACE2 could serve as a biomarker of the tissue ACE2, the researchers observed that the plasma ACE2 was not associated with ACE2 in any tissue. Despite an elevated plasma ACE2 linked with severe COVID-19 in clinical studies, the results observed here indicate that plasma ACE2 is not a suitable biomarker for tissue ACE2 in any tissue.
In the gender-specific study of ACE2 levels, the researchers found that ACE2 levels were higher in the kidneys of males than females. Previous studies have reported similar observations in mice without any drug treatment and in kidney tissue from human donors. This is the first report of sex differences in kidney ACE2 in mice treated with ACE inhibitor and ARB.
Limitations
The researchers pointed the major limitations of the study. Other ACE inhibitors or ARBs, apart from those used in the study, may have different effects on ACE2 abundance.
Because hypertension and cardiovascular disease can impact ACE2, the results observed in the healthy mice used in this study may be different in cardiovascular diseases.
While the observations found here are consistent with the available results in rats, the effects in humans may be different. Therefore, a similar controlled study in humans is essential.
Conclusions
This is the first study to
1) systemically evaluate the effect of ACE1 inhibition and angiotensin
receptor blockade on ACE2 protein abundance in tissue;
2) assess for gender-based differences in tissues; and
3) evaluate whether drug-induced changes in tissue ACE2 resolved after drug cessation.
While the lisinopril monotherapy increased the ACE2 protein in key tissues affected by SARS-CoV-2, the combination of lisinopril with losartan prevented the increase in ACE2 expression. This important study demonstrates that ACE inhibition and angiotensin receptor blockade interact to determine the tissue levels of ACE2.
*Important notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Brooks, S. et al. (2021) "Oral Lisinopril Raises Tissue Levels of ACE2, the SARS-CoV-2 Receptor, in Healthy Male and Female Mice", bioRxiv. doi: https://www.biorxiv.org/content/10.1101/2021.10.19.465025v1.full
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: ACE Inhibitors, ACE2, Allergy, Angiotensin, Angiotensin-Converting Enzyme 2, Assay, Biomarker, Blood, Blood Pressure, Brain, Cardiovascular Disease, Coronavirus, Coronavirus Disease COVID-19, Drugs, Enzyme, Gene, Gene Expression, Infectious Diseases, Kidney, Lisinopril, Losartan, Pathology, Preclinical, Protein, Receptor, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Small Intestine, Syndrome

Written by
Dr. Ramya Dwivedi
Ramya has a Ph.D. in Biotechnology from the National Chemical Laboratories (CSIR-NCL), in Pune. Her work consisted of functionalizing nanoparticles with different molecules of biological interest, studying the reaction system and establishing useful applications.
Source: Read Full Article
