Birth control is pretty damn important to lots of women—and, frankly, the easier it is to use, the better.
Sure, the Pill is fine and the ring gets the job done, but when you want some real, pregnancy-prevention staying power, it’s time to bring out the big guns: IUDs.
Remind me again, what are IUDs?
Intrauterine devices (IUDs) fall under the category of long-acting reversible contraceptives. This means that they prevent pregnancy for years but can be removed to restore fertility.
IUDs are 99 percent effective in protecting against pregnancy compared to 85 percent for condoms and 91 percent for the pill, according to Planned Parenthood. Basically, they are the best of both worlds: highly effective birth control you barely have to think about, says Sherry Ross, M.D., an ob-gyn and author of She-Ology: The Definitive Guide To Women’s Intimate Health. Period.
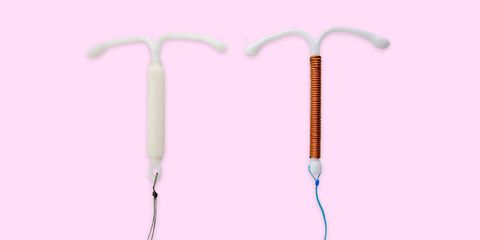
There are two categories of IUDs: hormonal and non-hormonal. There’s only one type of non-hormonal IUD—ParaGard. There are four hormonal IUDs currently approved by the FDA.

Most women are a good candidate for at least one type of IUD, though you’ll need to have a conversation with your doctor to figure out the best move, says Ross.
Sounds great, but um, aren’t IUDs painful?
All IUDs have the same basic look—again, plastic and T-shaped—and they’re all inserted through the cervix into your uterus. There are small strings on the end that protrude through the cervix into your vagina, letting you know that the IUD is still in place doing its thing.
Insertion, honestly, is different for everyone. For some women, especially those who’ve had children, it’s a minor annoyance; for others it can be extremely painful, particularly if the doctor needs dilators to open up your cervix more for insertion.
The good news is that the worst of it is over in a few minutes and the whole appointment shouldn’t take more than a half hour, says Ross. The bad news: While everyone’s different, there’s a chance that you could experience cramping or spotting for three to six months after insertion, according to Planned Parenthood. Removing it, thankfully, is usually pretty simple and pain-free, requiring a short doctor’s visit, she adds.
Here’s everything you need to know about the five different IUDs available right now:
1. ParaGard
How it works: Paragard is the only brand of non-hormonal IUD in the U.S. It’s wrapped in thin copper, which causes an inflammatory response in your body. This helps prevent sperm from getting through your cervix, and any little swimmers that do make it up there are neutralized by the copper ions, which are toxic to sperm.
Side effects: The inflammation caused by the copper blocks sperm, yes, but can also increase menstrual bleeding, both the duration and the flow, says Ross. Other side effects include anemia, increased cramps, and random spotting, she adds.
How long it lasts: According to ParaGard’s website, the device lasts for 10 years.
Who it’s best for: Women who want to avoid synthetic hormones for any reason, have a normal to light flow, and want the longest-lasting option.
Who should avoid it: If your cramps and bleeding are already bad, then a non-hormonal IUD probably isn’t for you, says Ross.
2. Mirena
How it works: Mirena releases 20 micrograms of levonorgestrel, a synthetic form of progesterone, per day. This hormone thickens your vaginal mucous, thins out your uterine lining, and can prevent your ovaries from releasing an egg, all of which prevent any rogue sperm from latching onto an egg and fertilizing it.
Side effects: Because it thins out your uterine lining, the most common side effect is having a significantly lighter period or no period at all, says Ross. Other issues may include nausea, breakthrough bleeding, ovarian cysts, and mood changes.
How long it lasts: Five years, according to Mirena’s website.
Who it’s best for: Women with super-heavy periods.
Who should avoid it: If you are prone to ovarian cysts or react badly to progestin, take a pass, says Ross, as Mirena could up your risk of those. If you’re hesitant about not having a period at all, skip this one, too.
3. Liletta
How it works: Liletta works exactly like the Mirena, except it uses slightly less levonorgestrel, releasing 19.5 micrograms per day—and that amount decreases a little each year after (that doesn’t hinder its effectiveness, though).
It was developed as a cheaper alternative to the Mirena (not all insurance plans cover IUDs). Women without health insurance can get Lilletta at a reduced cost through public-sector (a.k.a., free) clinics.
Side effects: Just like with Mirena, you may experience nausea, ovarian cysts, breakthrough bleeding, and mood changes. Many women also experience a lighter period or have no period at all.
How long it lasts: Four years, according to the Food and Drug Administration (FDA).
Who it’s best for: Women without health insurance or whose insurance doesn’t cover IUDs.
Who should avoid it: Women who react badly to synthetic progesterone or are prone to ovarian cysts should steer clear.
4. Kyleena
How it works: Kyleena works just like Mirena and Liletta but contains slightly less of the hormone levonorgestrel, releasing 17.5 micrograms a day—the second lowest dose you can find in a hormonal IUD.
Side effects: Again, this is similar to Mirena and Liletta, meaning side effects include nausea, ovarian cysts, breakthrough bleeding, and mood changes. It can also lessen or stop your period, but the effect isn’t as pronounced due to the smaller dosage.
How long it lasts: Five years, according to Kyleena’s website.
Who it’s best for: Women who still want ample protection, but also want to get their period regularly.
Who should avoid it: Women who react badly to synthetic hormones.
5. Skyla
How it works: Skyla works just like all four previously mentioned IUDs, but contains the smallest amount of levonorgestrel, releasing just 14 micrograms a day. It’s also the smallest in size, which means it may be easier to insert, particularly in women whose cervix is tighter, says Ross. (Worth noting: The size difference is pretty minimal.)
Side effects: The same as all the hormonal IUDs: cysts, nausea, mood swings, lighter bleeding. But because the dosage is lower, many women find the side effects to be less bothersome than IUDs with higher doses.
How long it lasts: Three years, per Skyla’s website.
Who it’s best for: Women who haven’t had children or have a tight cervix, or those who want to keep getting periods while they’re protected.
Who should avoid it: Women who would like protection for more than three years.
Source: Read Full Article
