The first case of concomitant visceral leishmaniasis and non-ulcerated cutaneous leishmaniasis in the same patient has been reported recently by researchers at the Federal University of São Carlos (UFSCar) in São Paulo state, Brazil, in an article published in the International Journal of Infectious Diseases.
The patient, a nine-year-old boy admitted to the hospital run by the Federal University of Sergipe (UFS), was infected by Leishmania infantum, a protozoan parasite that causes visceral leishmaniasis, and by another parasite of an as-yet unconfirmed species belonging to the genus Crithidia that causes symptoms similar to those of leishmaniasis, or even more severe symptoms in some cases.
In the Americas, Brazil is the country most affected by visceral leishmaniasis (VL), the most serious form of the disease, which can be lethal if it is not correctly treated or is misdiagnosed. The main agent of VL is L. infantum. Typical symptoms include weakness, weight loss, fever, an enlarged spleen and liver, and pancytopenia, i.e. low levels of all three blood cell types (red blood cells, white blood cells and platelets).
The advance of genomics in recent years has enabled researchers to find out that leishmaniasis patients can be co-infected with other genera of trypanosomatids in addition to Leishmania, such as Leptomonas and Crithidia, which in principle are not pathogenic to humans, or Trypanosoma, a genus of protozoan parasites that includes the agent of Chagas disease. Cases like these used to be associated with immunosuppression but are now seen in people with normal immune systems.
In 2019, the same group of researchers described a fatal case of a disease that was similar to VL but which they believed to be caused by a novel species of Crithidia, whereas C. fasciculata is known to infect only insects.
The report aroused controversy in the scientific community. Species of Leishmania are dixenous: their life cycle unfolds in two hosts, first in the vector (sandflies) and then in a human or other mammal. Crithidia are considered monoxenous, surviving only in one kind of host—typically mosquitoes or other insects.
The main alternative explanation presented at the time was that it could be a case of co-infection. The patient might have been infected by both Leishmania infantum and Crithidia, which is easily cultured in the laboratory and, if grown together with L. infantum, eliminates it from the culture.
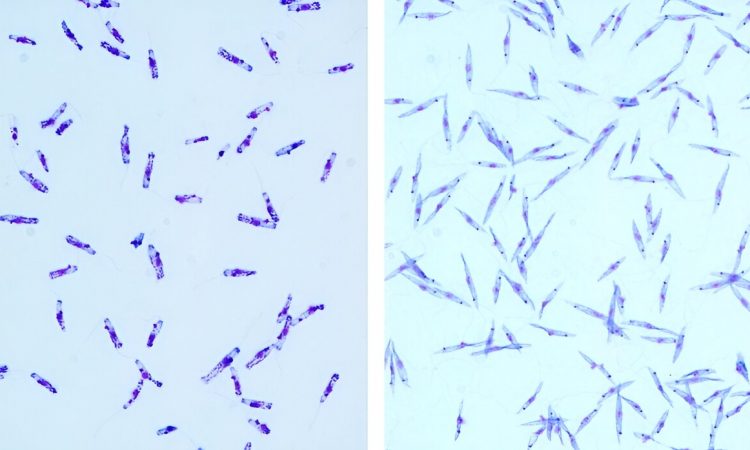
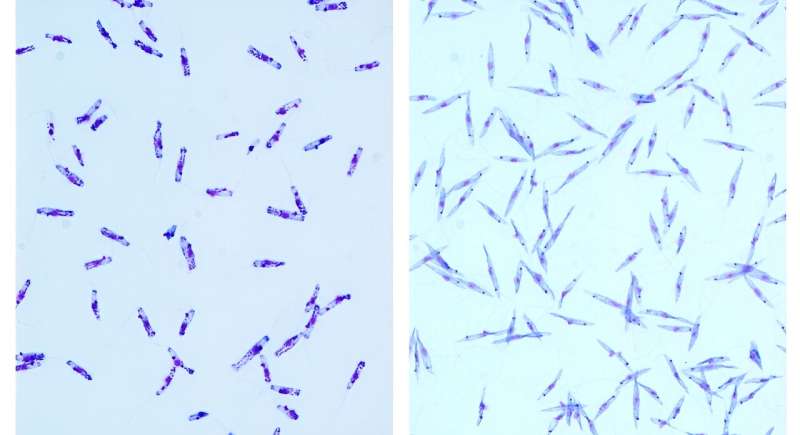
Co-infection was demonstrated in this latest study. Genome sequencing of bone marrow and spleen samples from the child hospitalized in Sergipe revealed the presence of both L. infantum and Crithidia. Furthermore, the child had a clinical manifestation not typical of VL, described as “non-ulcerated cutaneous leishmaniasis,” with nodular skin lesions from which L. infantum parasites were isolated.
The patient, who was monitored from 2016 to 2020 at the university hospital in Sergipe, had several VL relapses that did not respond to the available treatments, with clinical complications and a rare cutaneous manifestation concomitant with the visceral disease. During the fourth period of hospitalization, he underwent removal of his spleen and of a probable parasite reservoir.
Genomic sequencing of the parasites isolated from the patient suggested they were not in fact C. fasciculata, but another species that has yet to be named. “These results point to a series of novel hypotheses regarding not only the genus Crithidia, but also leishmaniasis itself,” said Sandra Regina Costa Maruyama, last author of the article.
Maruyama is a professor in UFSCar’s program of graduate studies in evolutionary genetics and molecular biology, and a researcher in its young investigator program.
“Which parasite caused the first infection? Did the patient already have severe leishmaniasis, so that he was more susceptible to infection by Crithidia? Or was Crithidia responsible for the primary infection, making the host more susceptible to infection by L. infantum?” Maruyama wondered.
“What about the vector for transmission of Crithidia to humans? Can the vector itself be co-infected by both parasites? We have many more questions than answers. It’s important to study infections by Crithidia in vertebrates and identify the possible vectors.”
Recent research in metagenomics of vector insects has shown that phlebotomine sandflies (the insects that transmit leishmaniasis) carry several microorganisms, such as viruses, bacteria and trypanosomatids, including Crithidia, Maruyama added.
Novel diagnostic target
VL is usually diagnosed on the basis of clinical symptoms, although several of its symptoms are common to other infectious diseases. Epidemiological features also contribute to the diagnosis. The main strategy currently used by public health services in the SUS (Sistema Único de Saúde, Brazil’s national health network) is a quick test to detect antibodies against Leishmania rather than the parasite itself.
This is practical but not as highly specific as molecular methods that directly detect the presence of the protozoan in the sample. More precise differentiation of L. infantum and the species of Crithidia during the study was therefore crucial. The researchers developed a molecular method specifically to detect these species. The recent article outlines the method, and more details will be provided in a forthcoming article.
“We managed to find the same species of Crithidia in samples from several other VL patients,” Maruyama said.
Public health
Besides investigating the possible new Crithidia species to confirm whether it is indeed an emerging parasite capable of having an impact in Brazil, the next step for the researchers will be to analyze the effects of co-infection, especially whether it aggravates VL.
“We know only a small proportion of patients who test positive for infection by Leishmania develop the disease. However, the tests are serological and the two types of parasite have very similar proteins, so it’s impossible to distinguish between them in order to be sure which is the infecting species,” Maruyama said.
The importance of finding out more and understanding the novel component is even greater in view of the advance of VL in Brazil. “VL used to be concentrated in the Northeast [the region where Sergipe is located], but cases of the disease are now reported even in the South. The situation is critical in Minas Gerais state. Experts have warned us about the advance of the disease in São Paulo state,” she said.
More information:
Luana Aparecida Rogerio et al, Co-infection of Leishmania infantum and a Crithidia-related species in a case of refractory relapsed visceral leishmaniasis with non-ulcerated cutaneous manifestation in Brazil, International Journal of Infectious Diseases (2023). DOI: 10.1016/j.ijid.2023.05.012
Journal information:
International Journal of Infectious Diseases
Source: Read Full Article