Researchers at the German Center for Neurodegenerative Diseases (DZNE) and the Institute for Stroke and Dementia Research (ISD) at the LMU Medical Center have found that a protein named TREM2 may have a mitigating effect on the course of Alzheimer’s disease. In a new study led by Professor Christian Haass (LMU, DZNE) and Professor Michael Ewers (ISD, LMU), patients who have higher levels of TREM2 in their cerebrospinal fluid (CSF) at various stages of the disease have a better prognosis than those in whom the protein is present in lower amounts. This observation provides a starting point for the development of new therapeutic strategies. The study appears in the latest issue of the journal Science Translational Medicine.
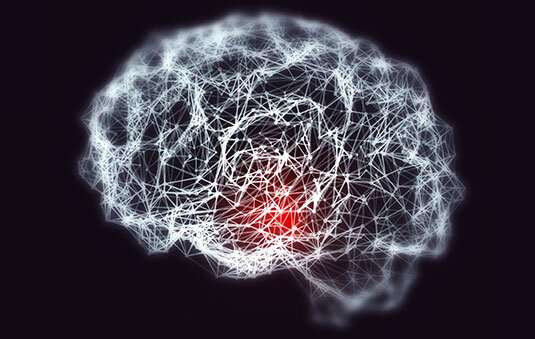
In the brain, TREM2 is produced exclusively by the microglia, which serve as the organ’s immune cells. These cells patrol the brain, disposing of cellular waste products and abnormal extracellular deposits. Earlier studies carried out by Haass and his colleagues in mice had shown that TREM2 activates microglia to enclose and selectively destroy toxic protein aggregates typical for Alzheimer’s disease. These observations suggested that TREM2 might protect the brain from the degenerative effects of Alzheimer’s—at least in the mouse model. But can these results be extended to Alzheimer patients? Does TREM2 also have a protective effect in the human brain? In earlier work, teams led by Haass and Ewers had also shown that the concentration of TREM2 is elevated in samples of CSF obtained from Alzheimer patients, most probably as a result of the activation of microglia in response to the pathological changes associated with the condition. However, the crucial issue remained unresolved: Do higher levels of TREM2 represent a protective or a deleterious response to these changes?
In order to answer this question, Ewers, Haass and their colleagues set out to establish a statistical correlation between the concentration of TREM2 in the CSF samples from their patient population and the rate of disease progression in these individuals over several years. They made use of data for 385 patients, collected by the “Alzheimer’s Disease Neuroimaging Initiative” (ADNI), a large clinical dataset comprising medical records and samples obtained not only from Alzheimer patients, but also from healthy seniors taken at regular checkups for many years. These data should make it possible to discern any meaningful associations between specific biochemical changes and the clinical course of Alzheimer’s.
Indeed Ewers and Haass were able to confirm that higher concentrations of TREM2 are linked to a more favorable prognosis at all stages of the disease. In these subjects, memory was less unstable and the rate of shrinkage of the hippocampus—a region of the brain that plays a vital role in learning and memory ¬– was less pronounced. “Our findings are of clinical relevance, because these patients displayed a consistently reduced risk of developing dementia over a period of 11 years,” says Ewers. “However, activation of the microglia is a double-edged sword. In addition to providing protective effects, it can lead to inflammation processes. Nevertheless, TREM2 could play a key role in triggering a protective immune response in the brains of patients with Alzheimer’s disease.”
Source: Read Full Article
